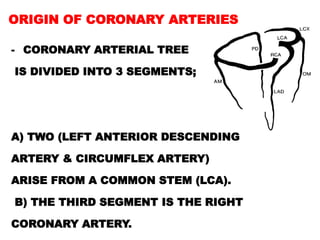
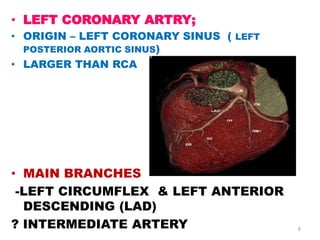
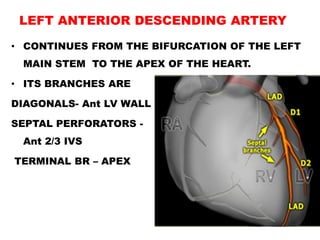
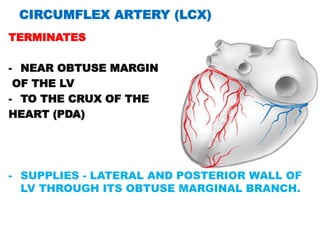
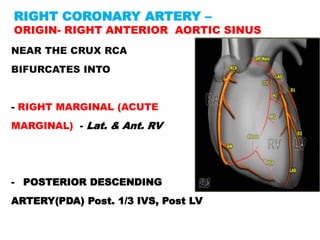
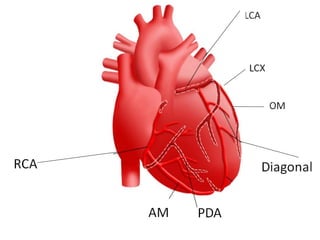
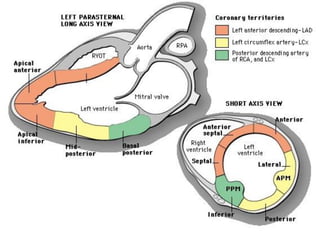
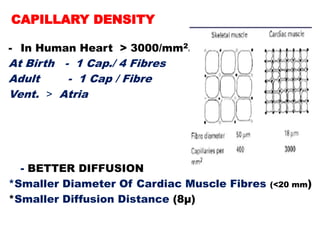
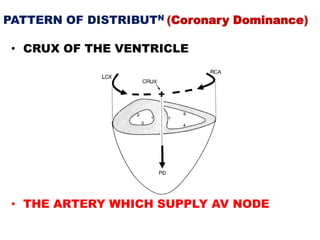
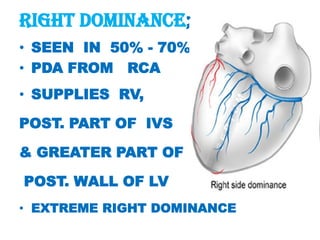
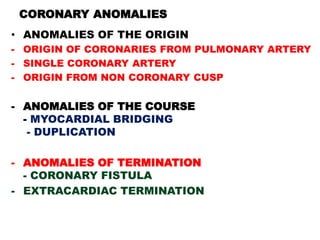
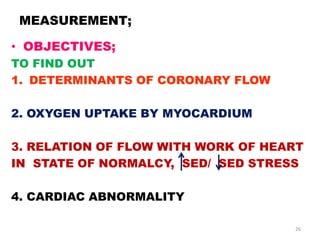
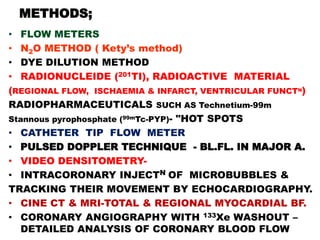
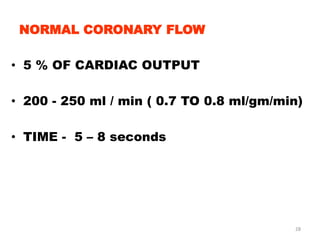
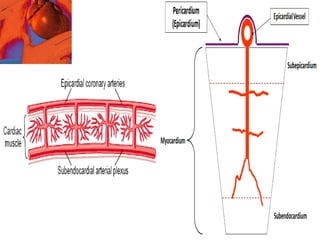
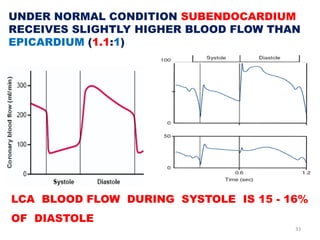
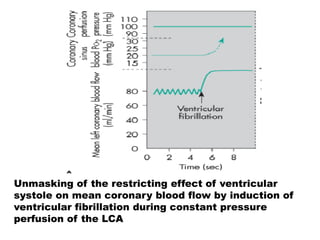
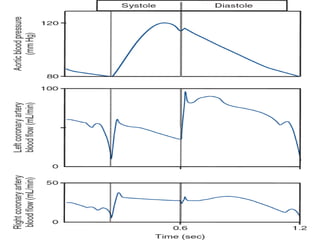
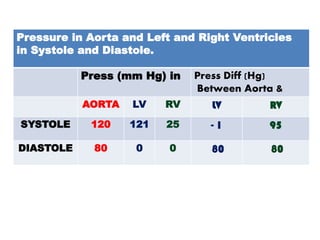
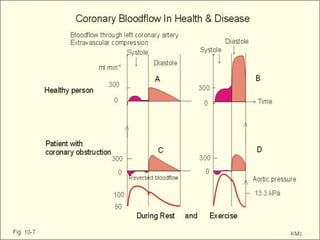
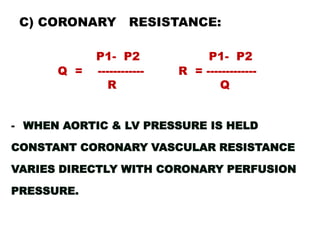
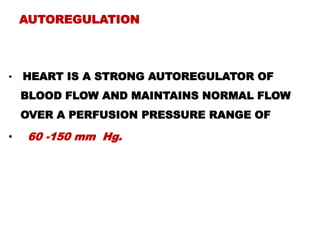
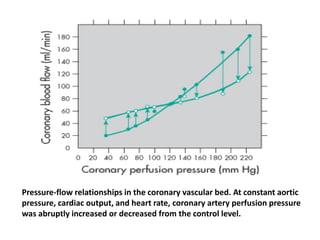
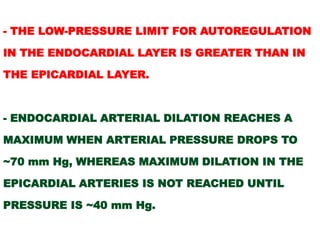
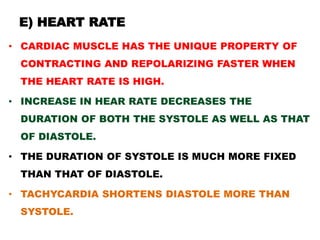
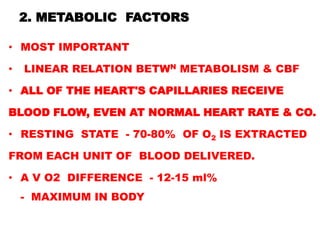
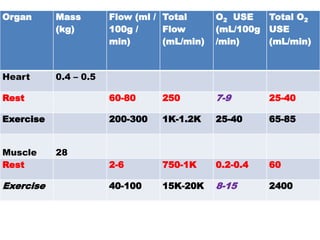
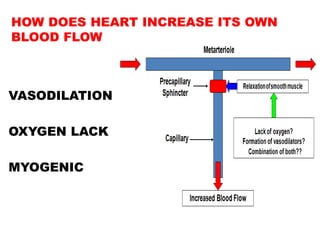
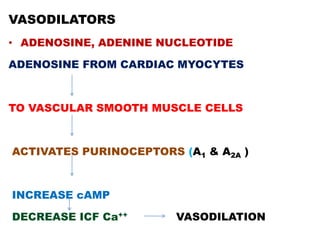
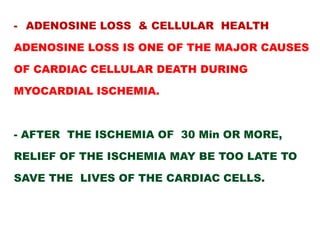
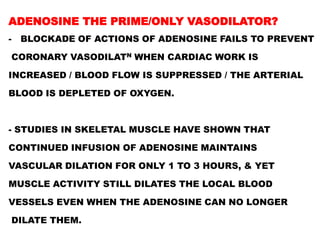
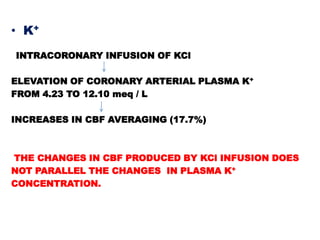
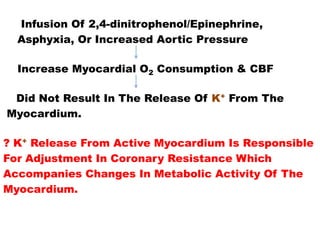
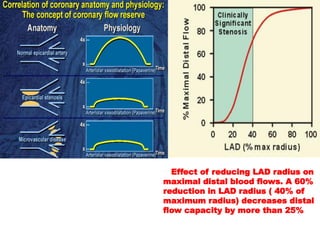
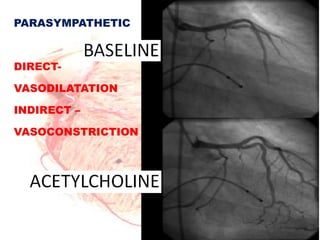
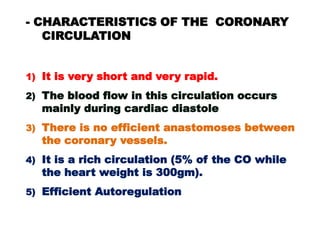
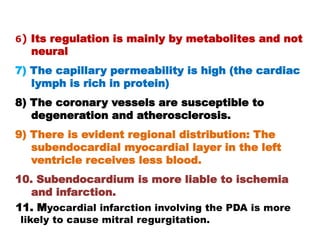
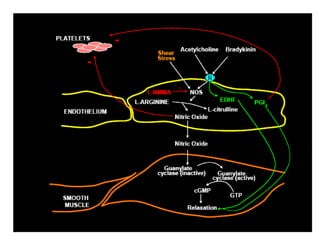
This document discusses coronary circulation and the factors that influence coronary blood flow. It provides details on the physiologic anatomy of the coronary arteries, including their origin, branches, and distribution. It also discusses the normal coronary blood flow and various physical, metabolic, neural, and neurohormonal factors that can impact coronary flow, such as cardiac cycle, aortic pressure, coronary resistance, heart rate, and myocardial metabolism. The document emphasizes the critical role of metabolic factors and how the heart regulates its own blood flow in response to oxygen demand.