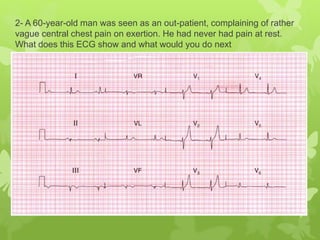
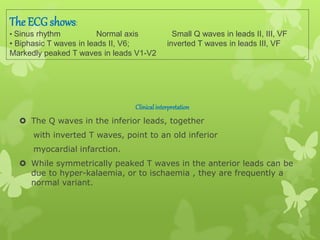
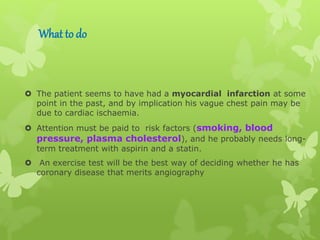
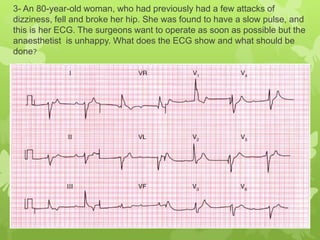
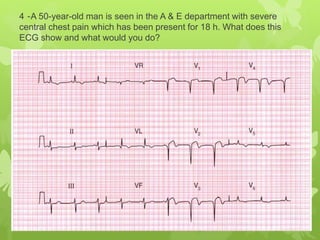
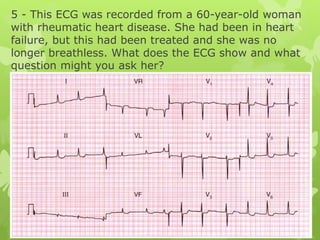
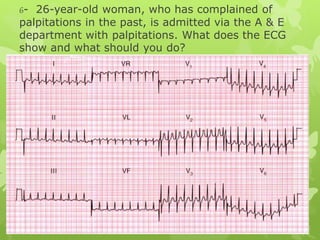
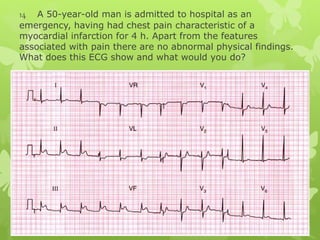
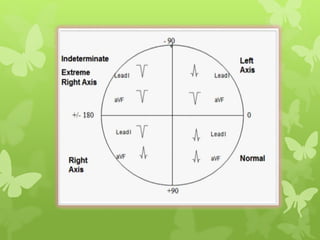
This document contains 6 ECG readings from patients presenting with various chest complaints. For each reading, it provides the clinical interpretation of the ECG findings and recommends next steps in management, such as administering thrombolytics, referring for angiography, or implanting a pacemaker. Common presentations included prior heart attacks, heart block, acute myocardial infarction, and supraventricular tachycardia. The recommended treatments were aimed at addressing the underlying cardiac issues and providing symptom relief.