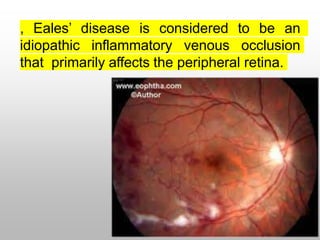
Eales' disease is an idiopathic inflammatory retinal condition that primarily affects veins in the retina. It is characterized by perivascular inflammation that can lead to retinal ischemia and neovascularization. The disease progresses through stages from inflammation to ischemia to proliferation of new blood vessels. Treatment involves corticosteroids to reduce inflammation, laser photocoagulation to ablate new vessels, and vitrectomy for complications like vitreous hemorrhage or retinal detachment. While the exact cause is unknown, hypersensitivity to tuberculosis has been proposed as a potential trigger in many cases.