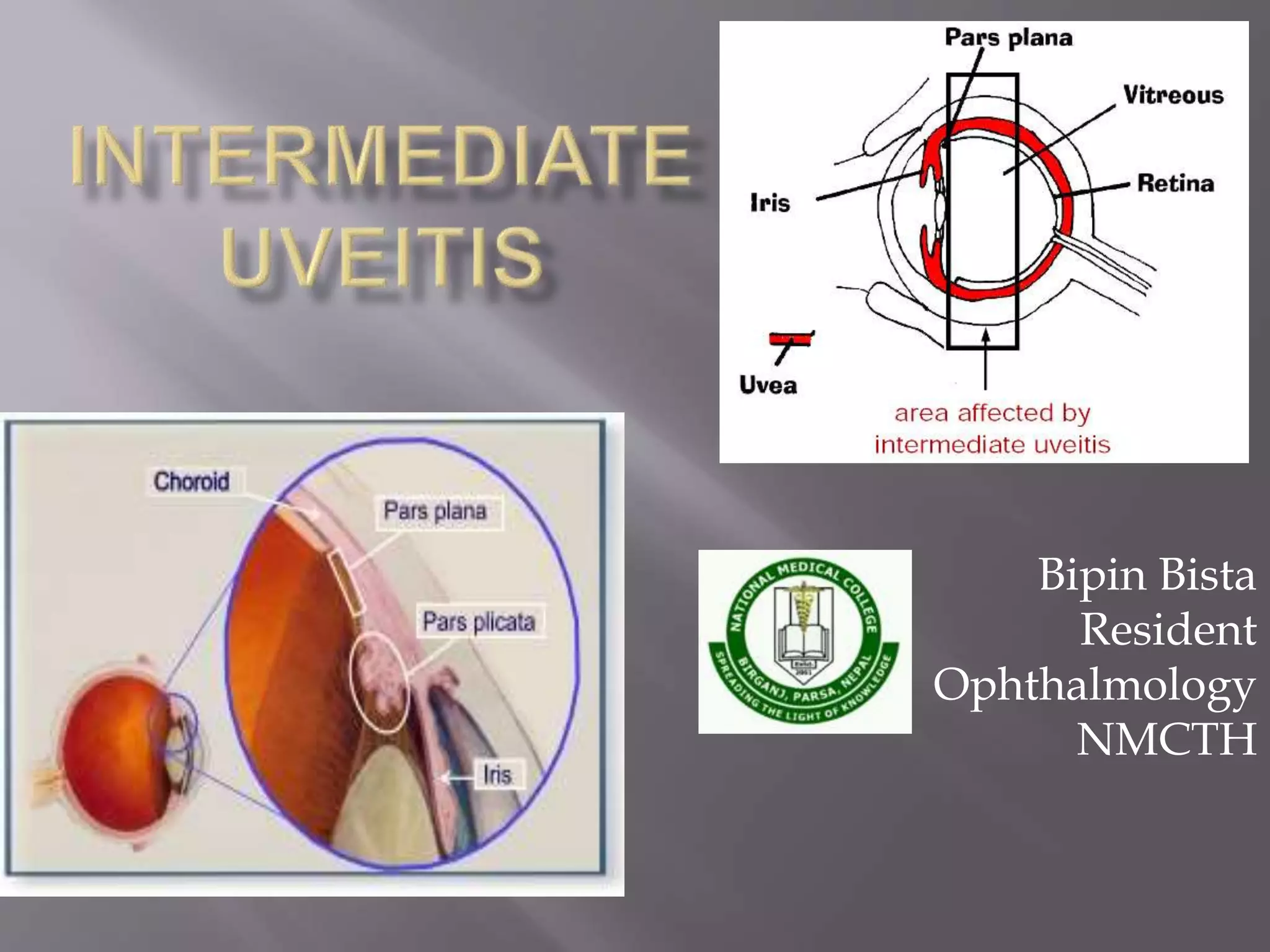
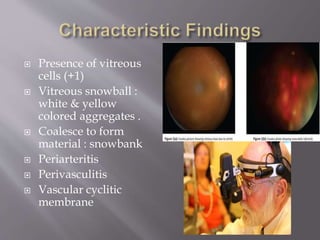
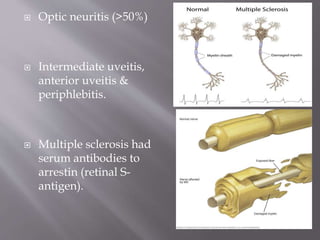
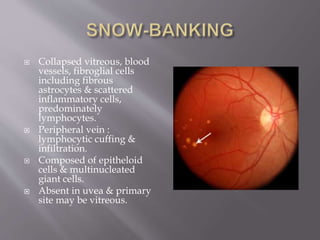
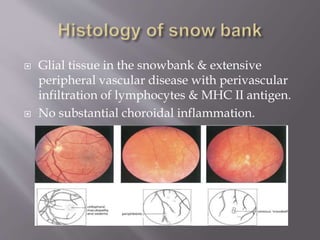
Intermediate uveitis is characterized by inflammation of the vitreous and peripheral retina. Symptoms include blurred vision, floaters, and decreased visual acuity. If left untreated, it can cause severe visual loss or sudden vision loss. Diagnosis is made based on the presence of vitreous cells and snowball or snowbank formations in the vitreous. Treatment involves systemic corticosteroids or immunosuppressive drugs to reduce inflammation. Additional treatments may include periocular corticosteroid injections, cryotherapy, or vitrectomy.