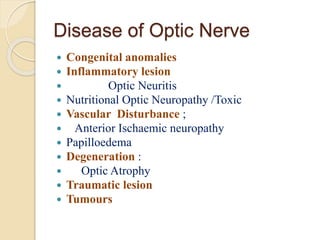
This document discusses optic nerve disease and optic neuropathy. It covers the clinical features, examination, investigations, and various causes of optic nerve disease including optic neuritis, nutritional optic neuropathy, anterior ischemic optic neuropathy, papilledema, and Leber's hereditary optic neuropathy. Examinations discussed include visual acuity testing, color vision testing, visual field testing, ophthalmoscopy, fluorescein angiography, and visual evoked potentials. Causes covered in more depth include optic neuritis, anterior ischemic optic neuropathy, nutritional optic neuropathy, papilledema, and Leber's hereditary optic neuropathy.