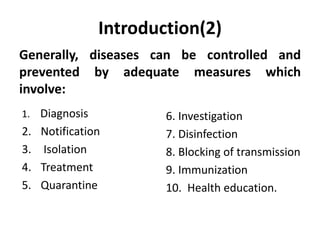
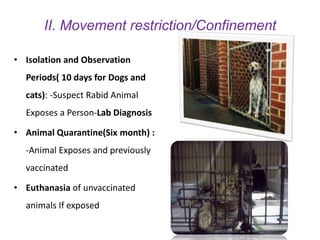
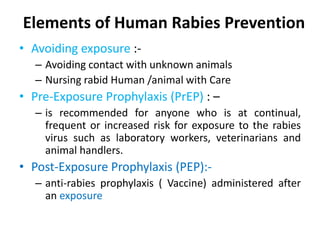
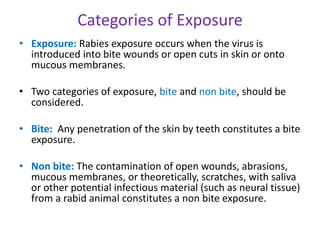
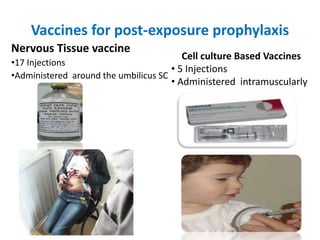
This document outlines measures for rabies prevention and control, including animal and human components. Animal rabies control involves mass dog vaccination, movement restrictions, and stray dog control. Human prevention includes avoiding animal exposures, pre-exposure vaccination for high-risk groups, and post-exposure prophylaxis consisting of wound treatment, vaccination, and possibly rabies immunoglobulin. Effective rabies prevention and control requires legal frameworks, adequate resources, expanded diagnostics, collaboration among stakeholders, and community education.