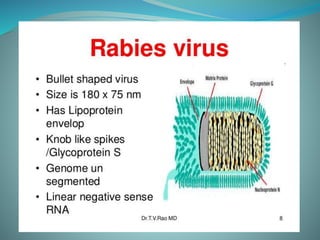
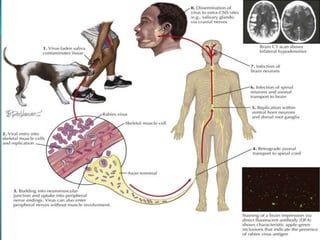
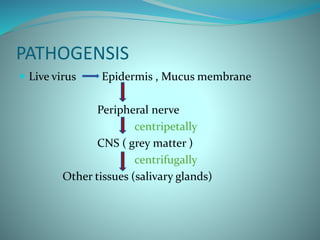
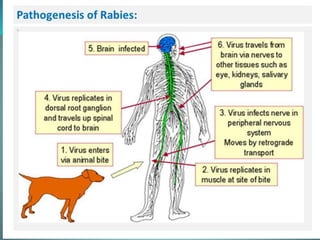
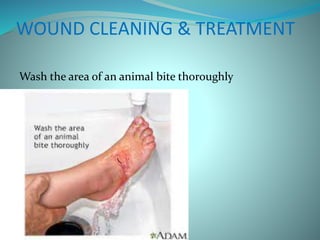
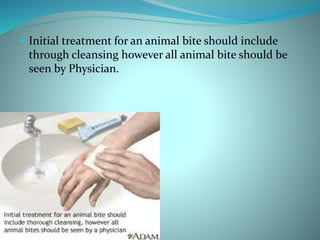
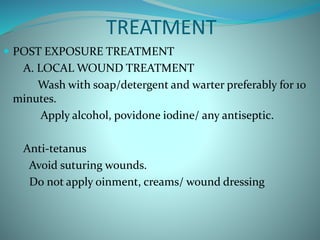
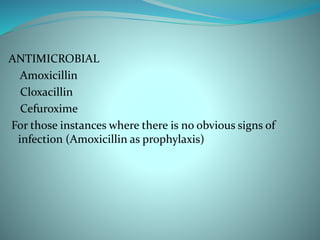
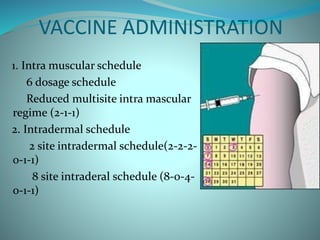
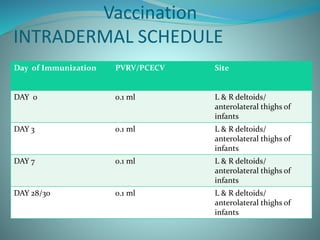
Rabies is a viral disease causing acute encephalitis in warm-blooded animals, primarily transmitted to humans through bites or scratches from infected animals, mostly dogs. Symptoms include bizarre behavior, hydrophobia, and paralysis, with a high fatality rate once they develop, necessitating immediate treatment including wound care and vaccinations. Prevention involves pre-exposure and post-exposure prophylaxis, with attention to timely management and infection control in cases of confirmed rabies.