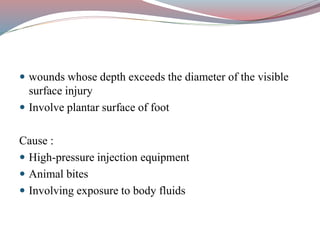
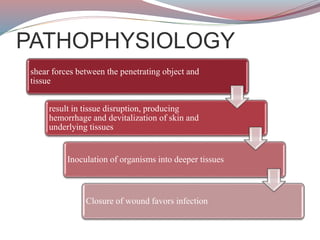
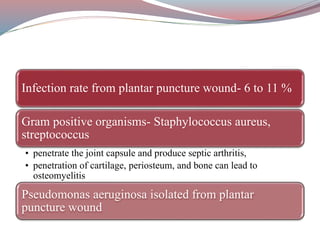
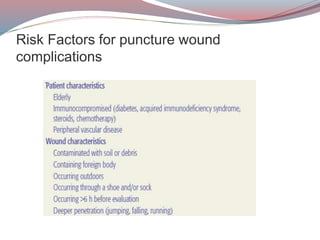
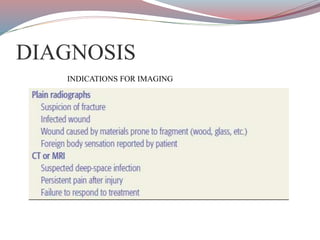
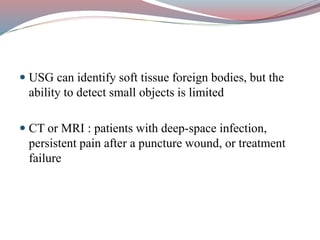
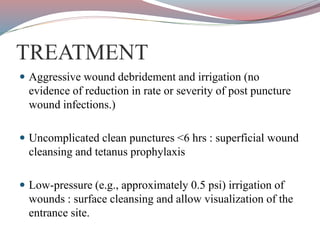
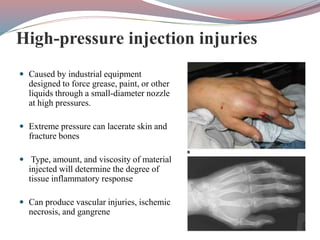
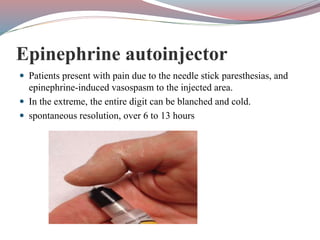
This document provides information on puncture wounds and their management. It discusses the pathophysiology, risk factors, clinical features, diagnosis, and treatment of various types of puncture wounds including those from high pressure injection injuries, animal bites, needle sticks, and more. Complications are outlined along with prevention and management recommendations. Imaging, wound care, debridement, antibiotics, and tetanus prophylaxis are frequently recommended depending on the wound type and risk of infection.