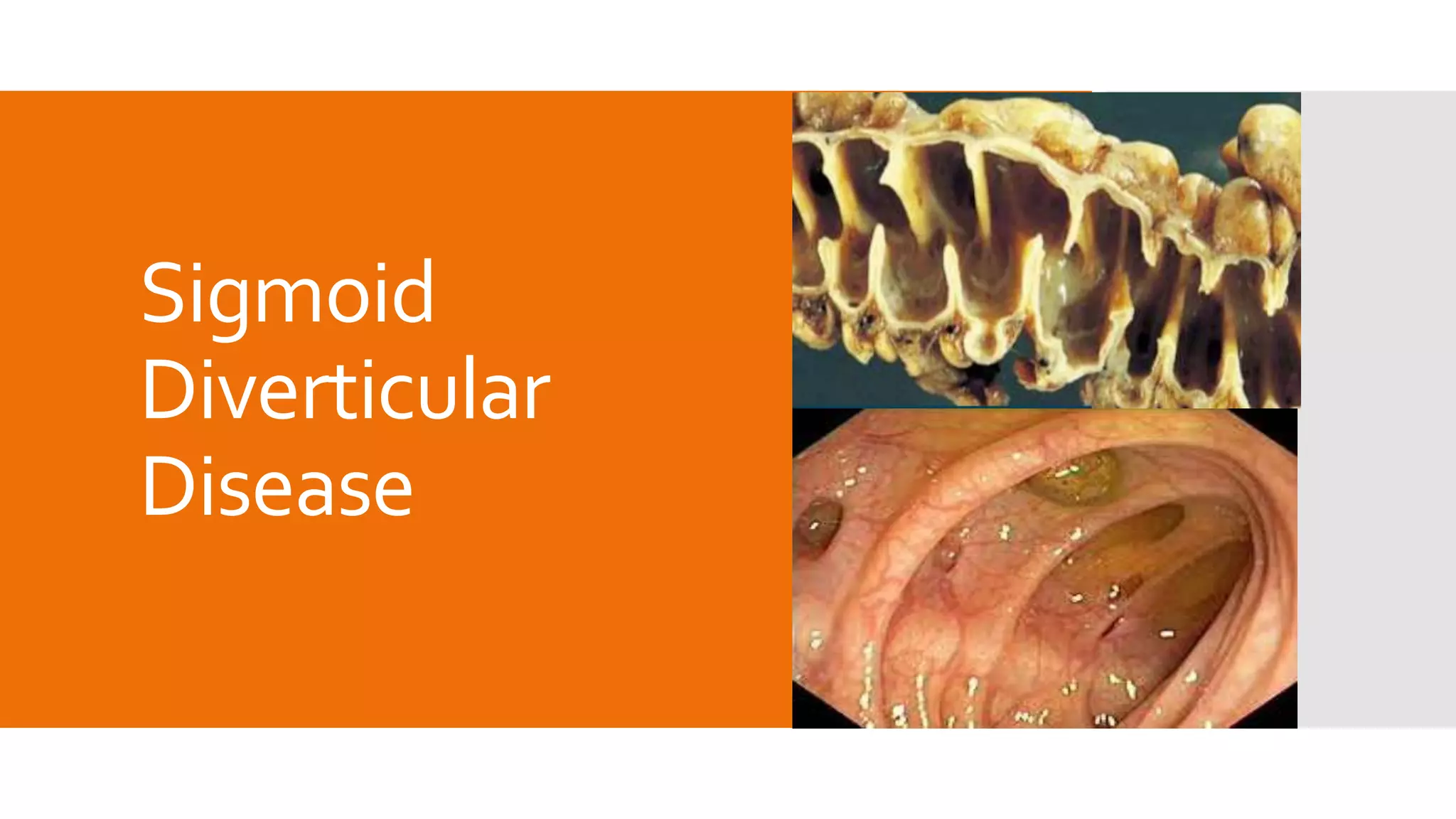
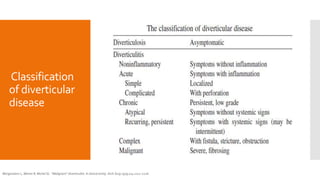
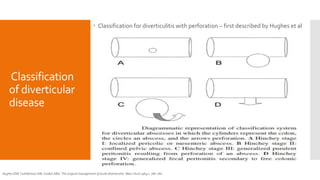
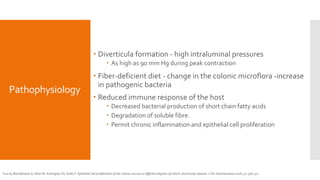
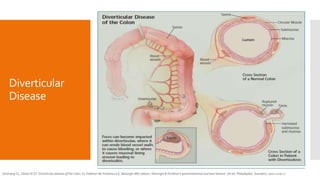
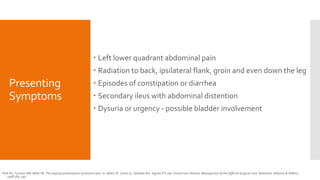
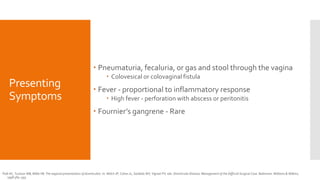
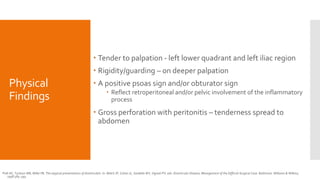
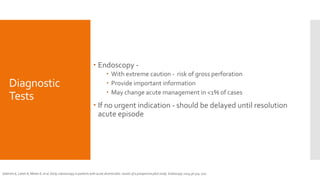
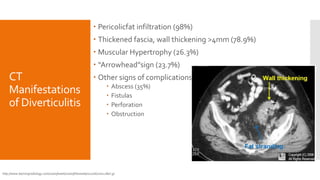
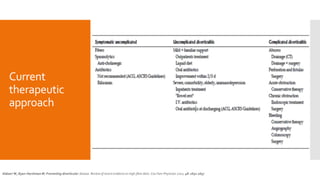
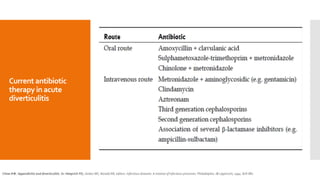
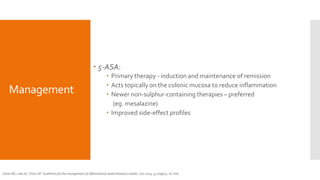
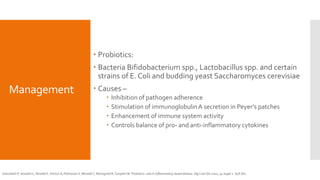
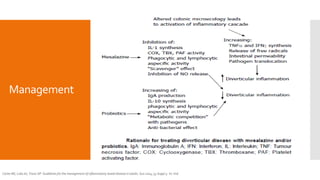
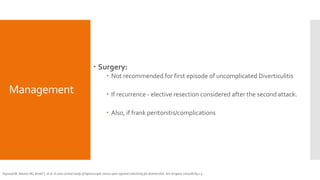
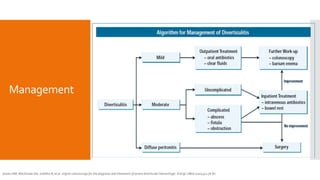
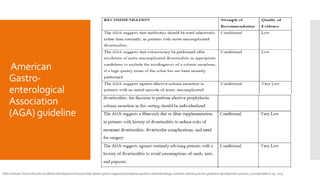
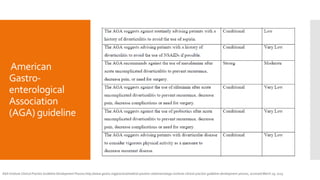
This document provides a comprehensive overview of sigmoid diverticular disease, including its pathophysiology, classification, symptoms, diagnosis, and management. It highlights the increasing prevalence of diverticular disease in industrialized societies and discusses various diagnostic methods such as CT scans and imaging techniques. Management strategies range from dietary modifications and medical therapies to surgical interventions for recurrent cases, with ongoing research aimed at improving treatment outcomes.