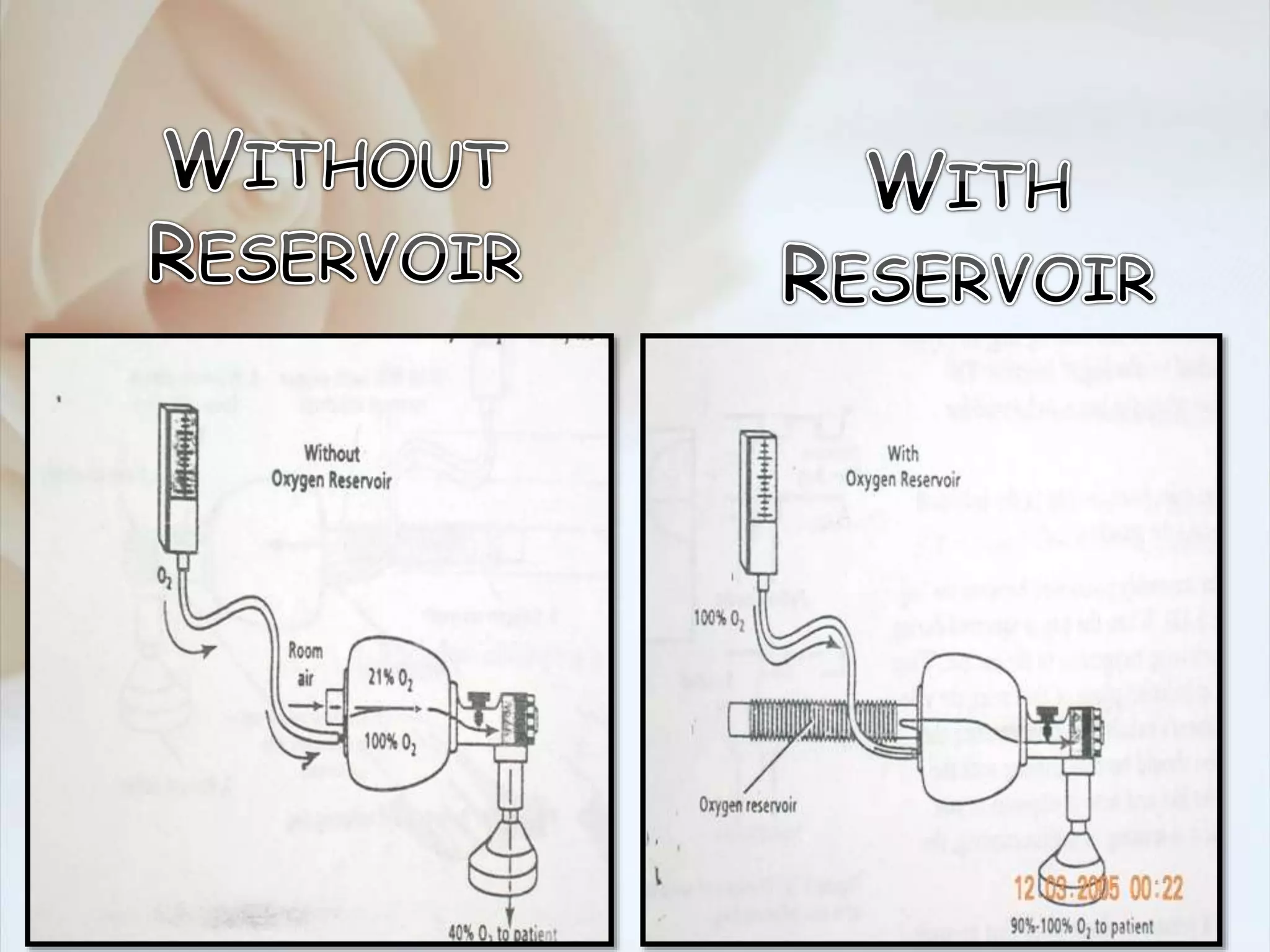
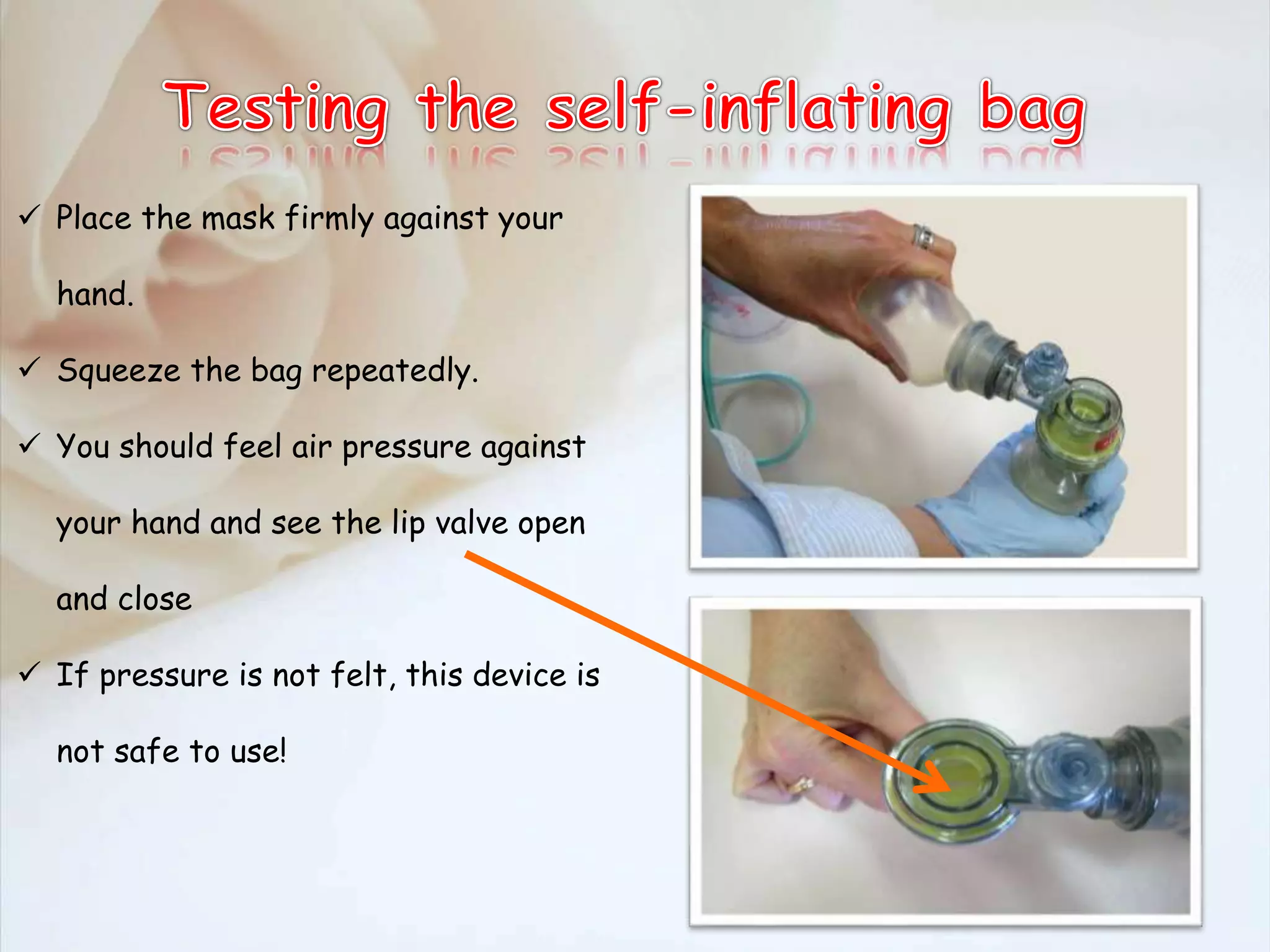
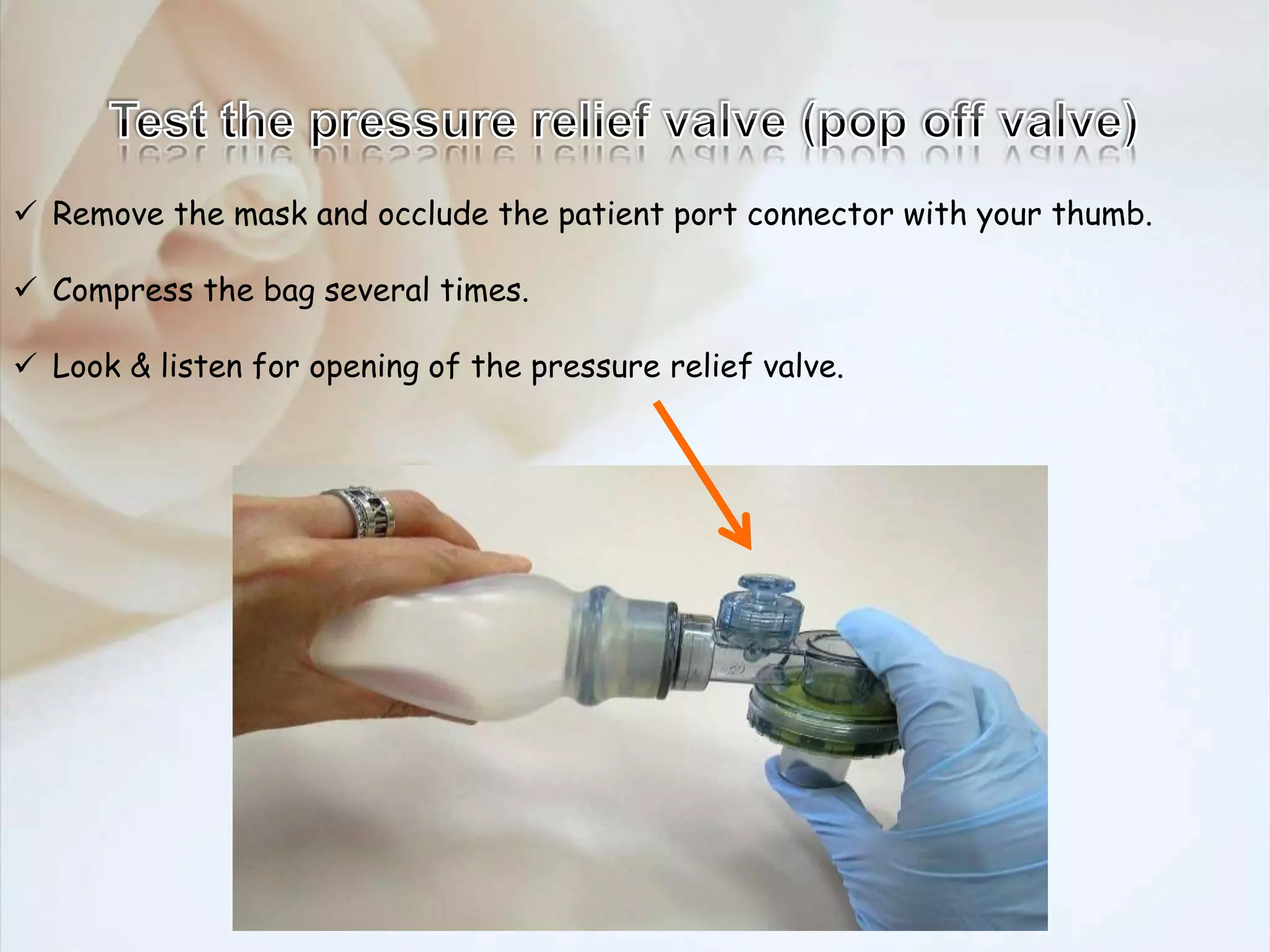
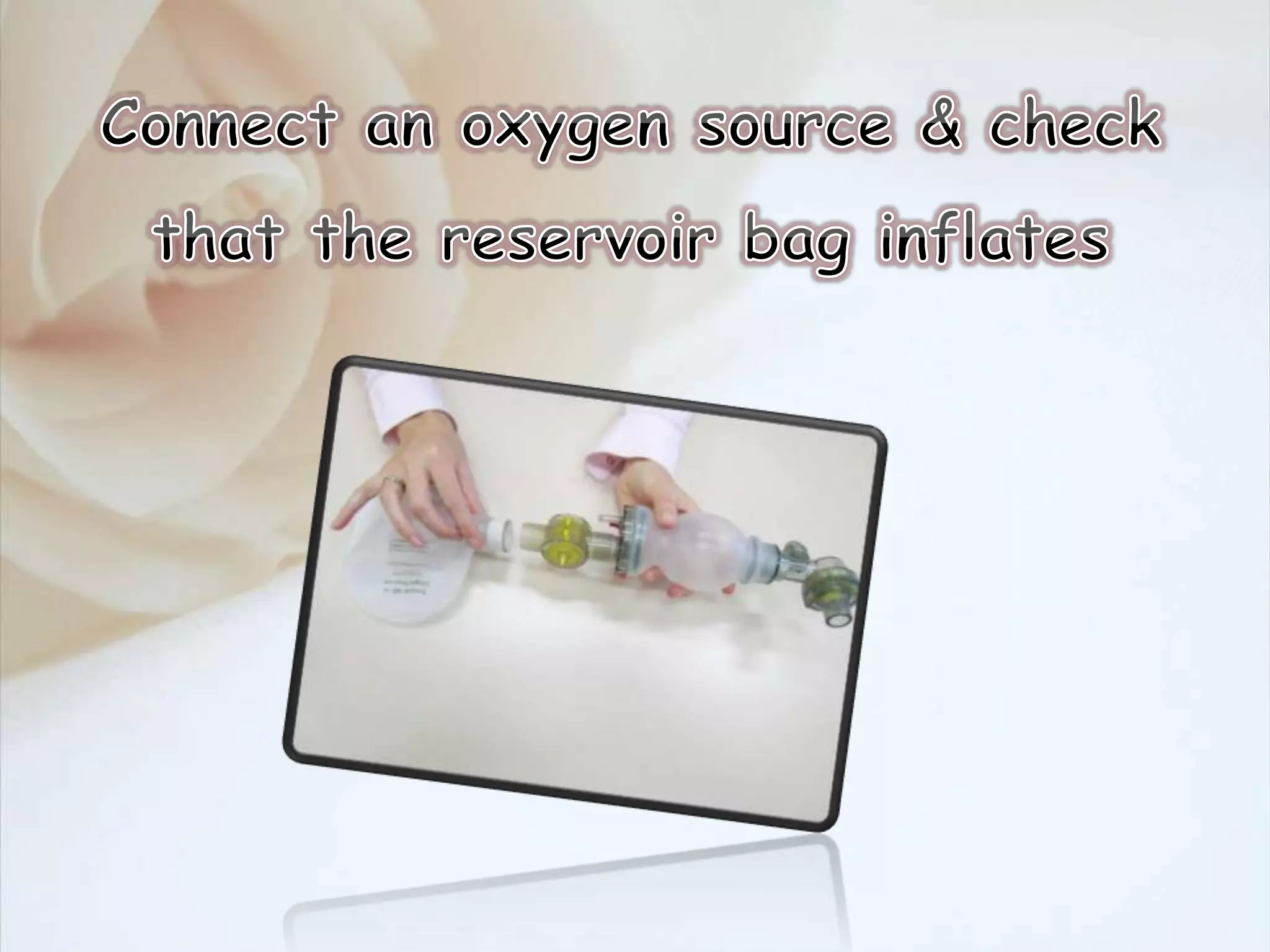
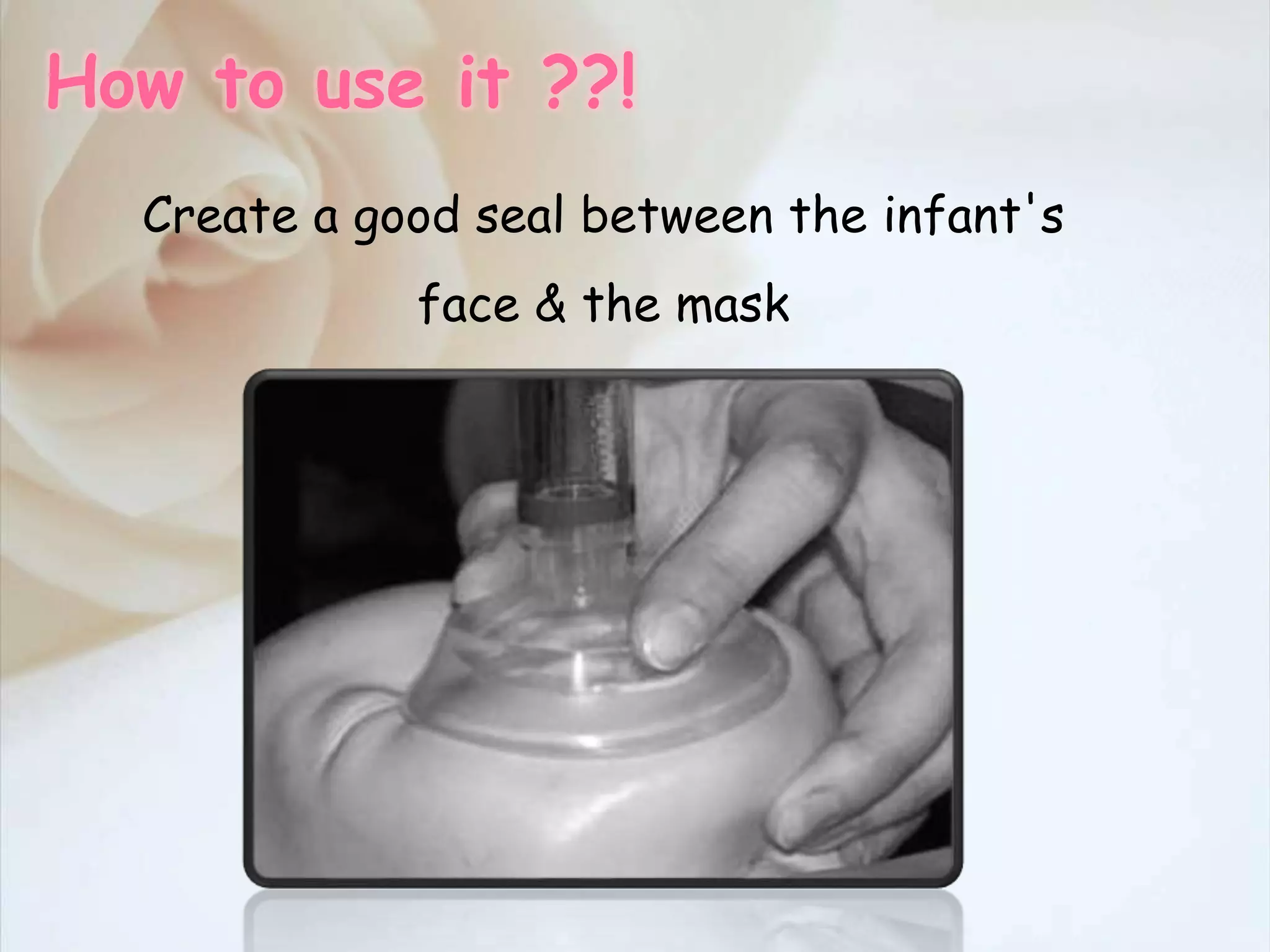
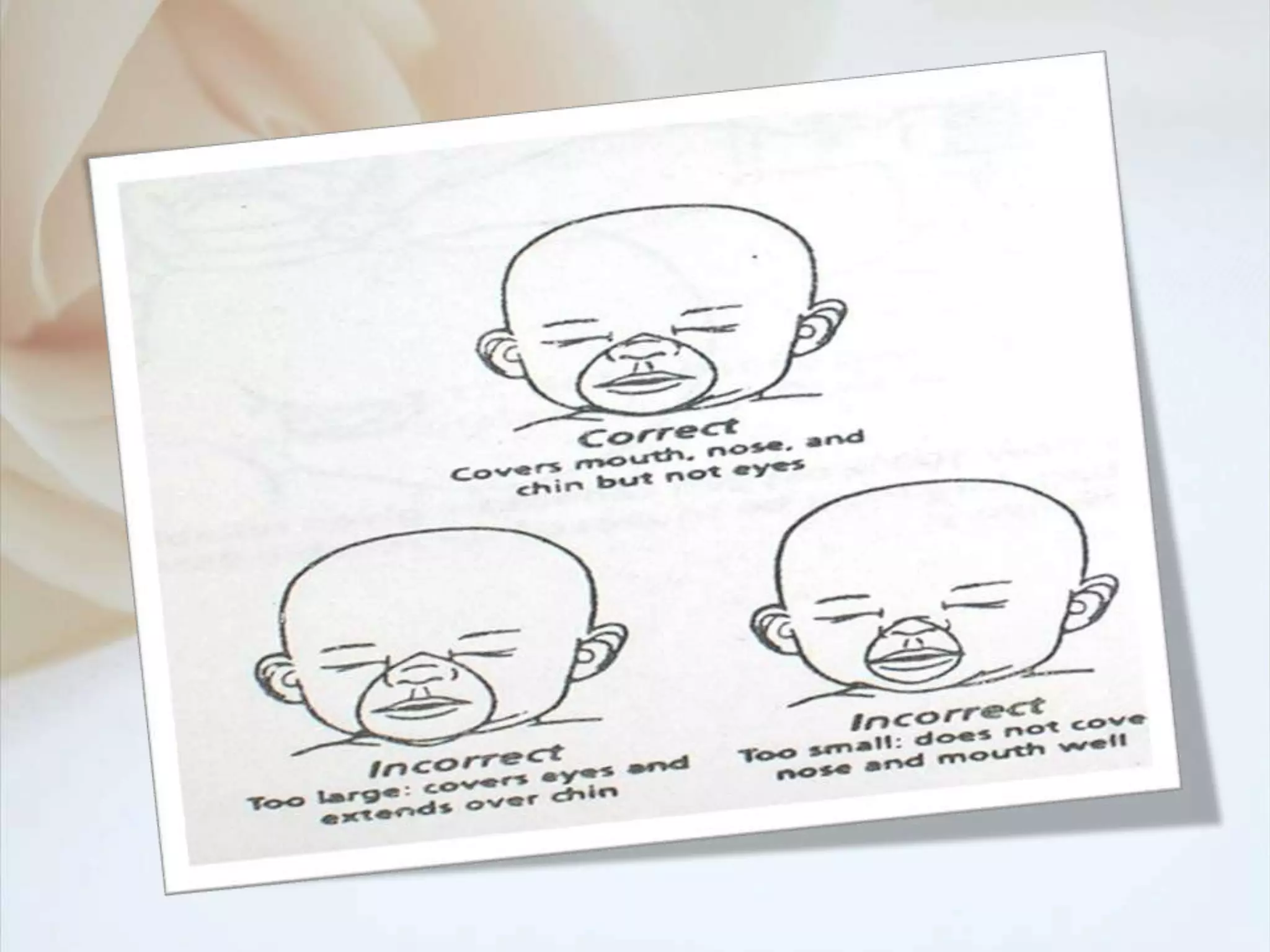
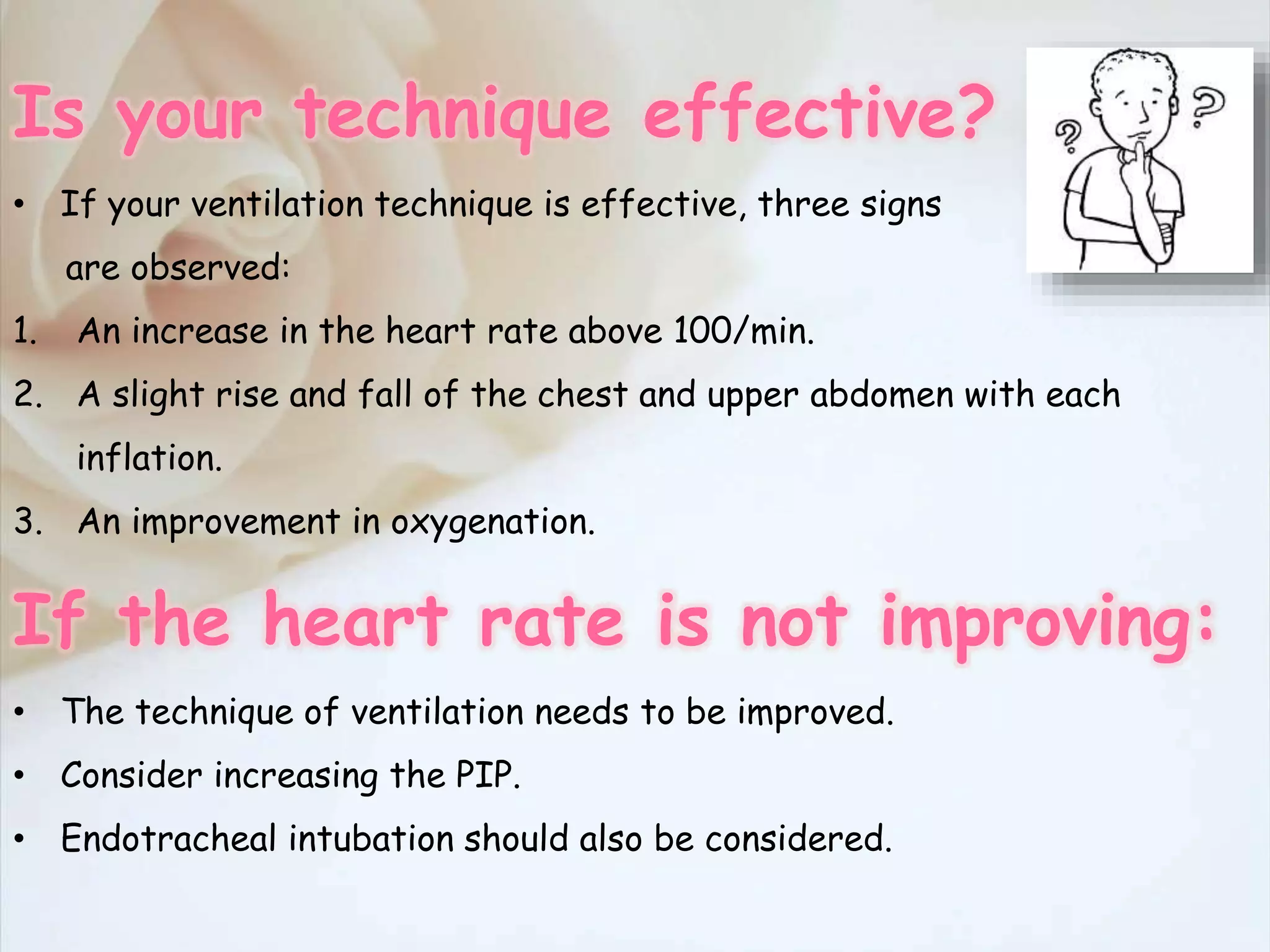
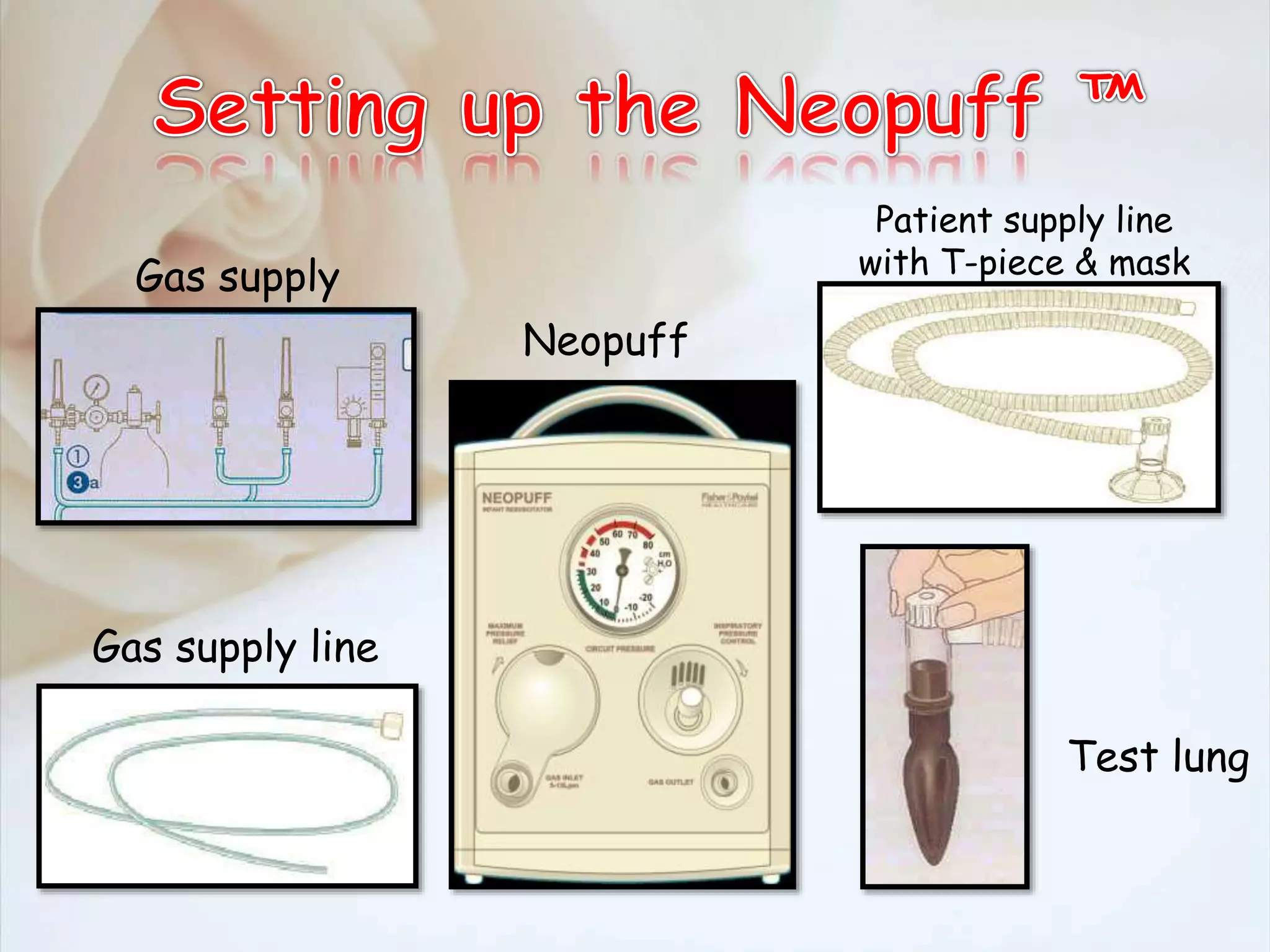
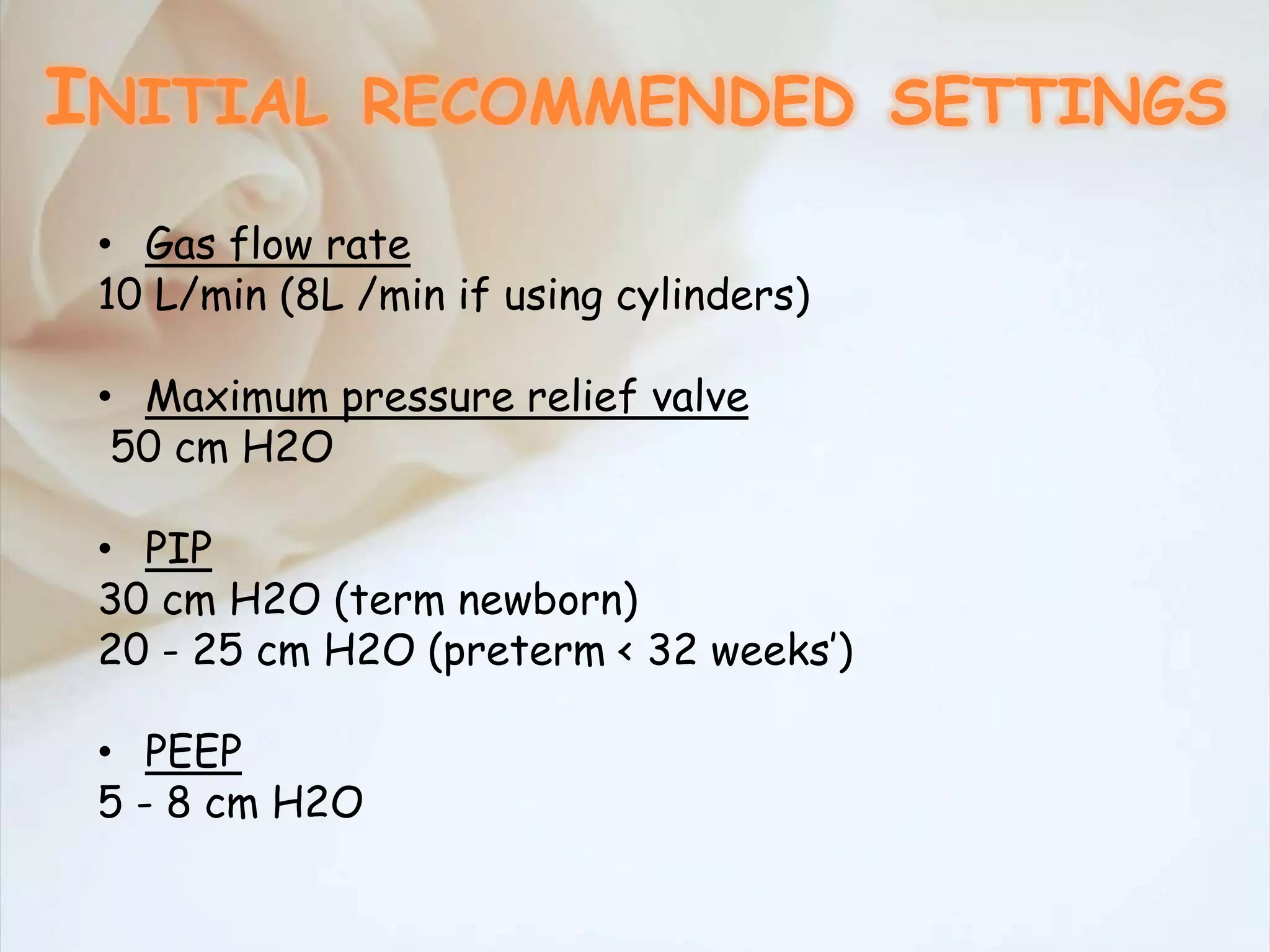
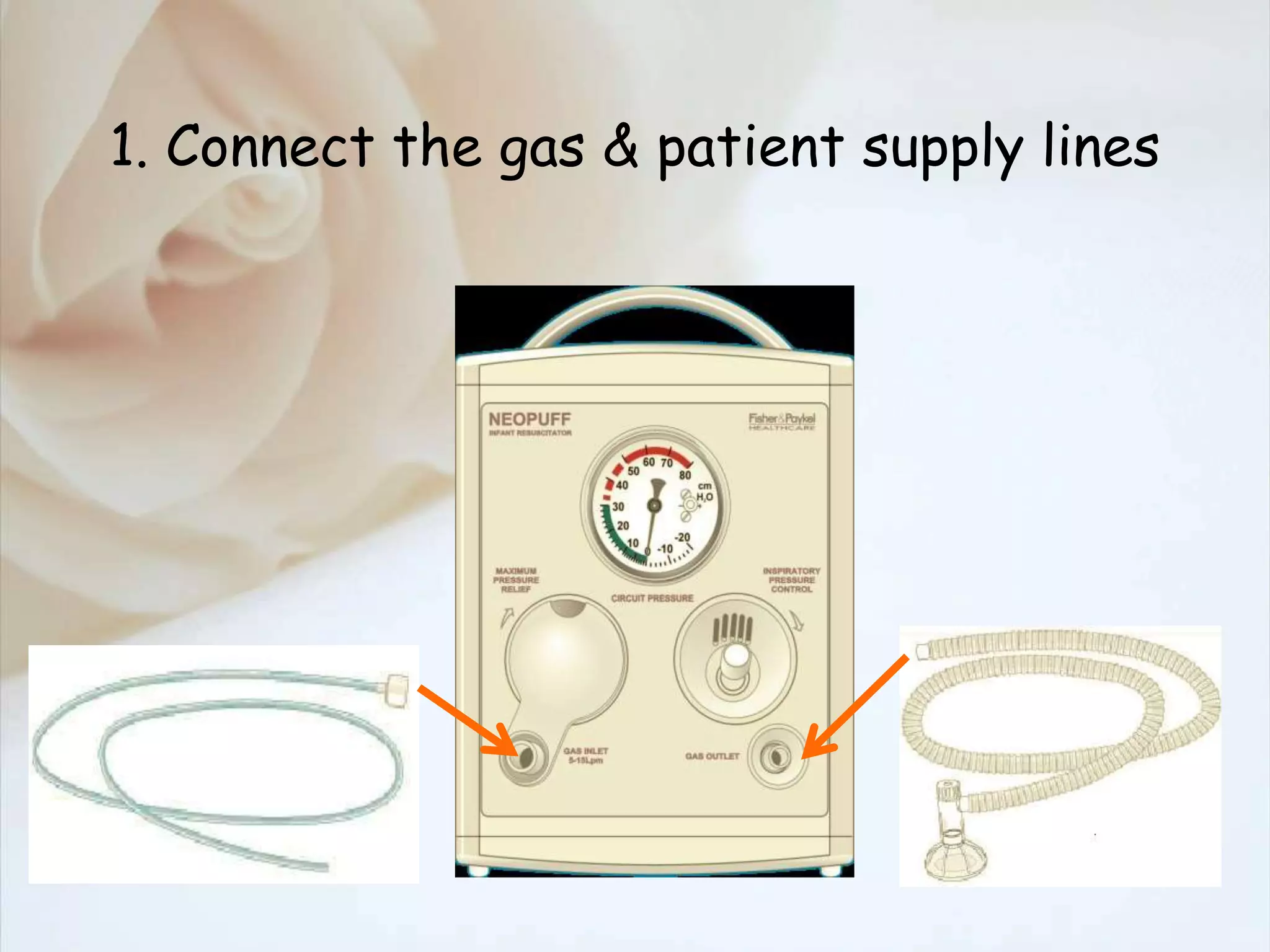
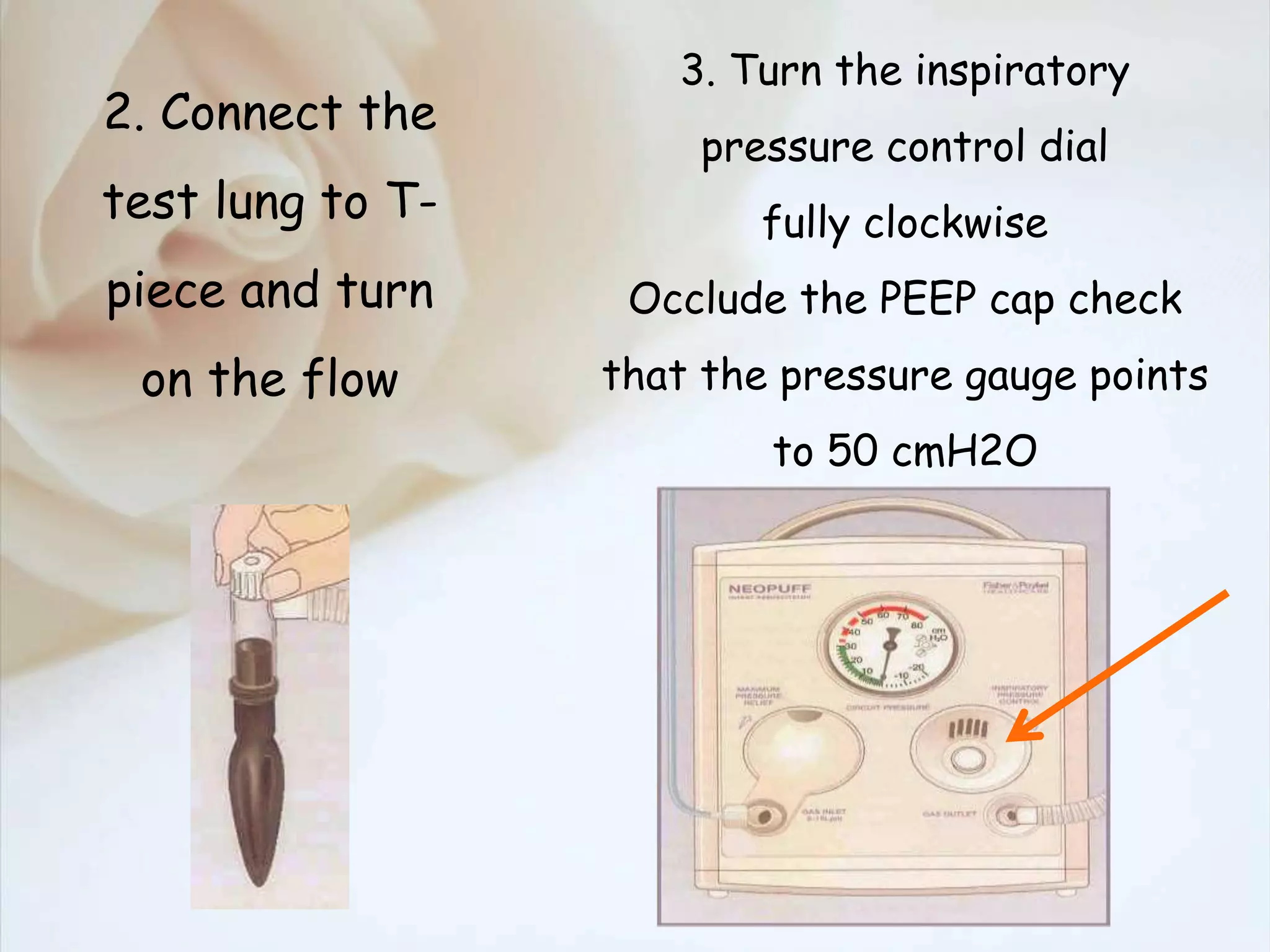
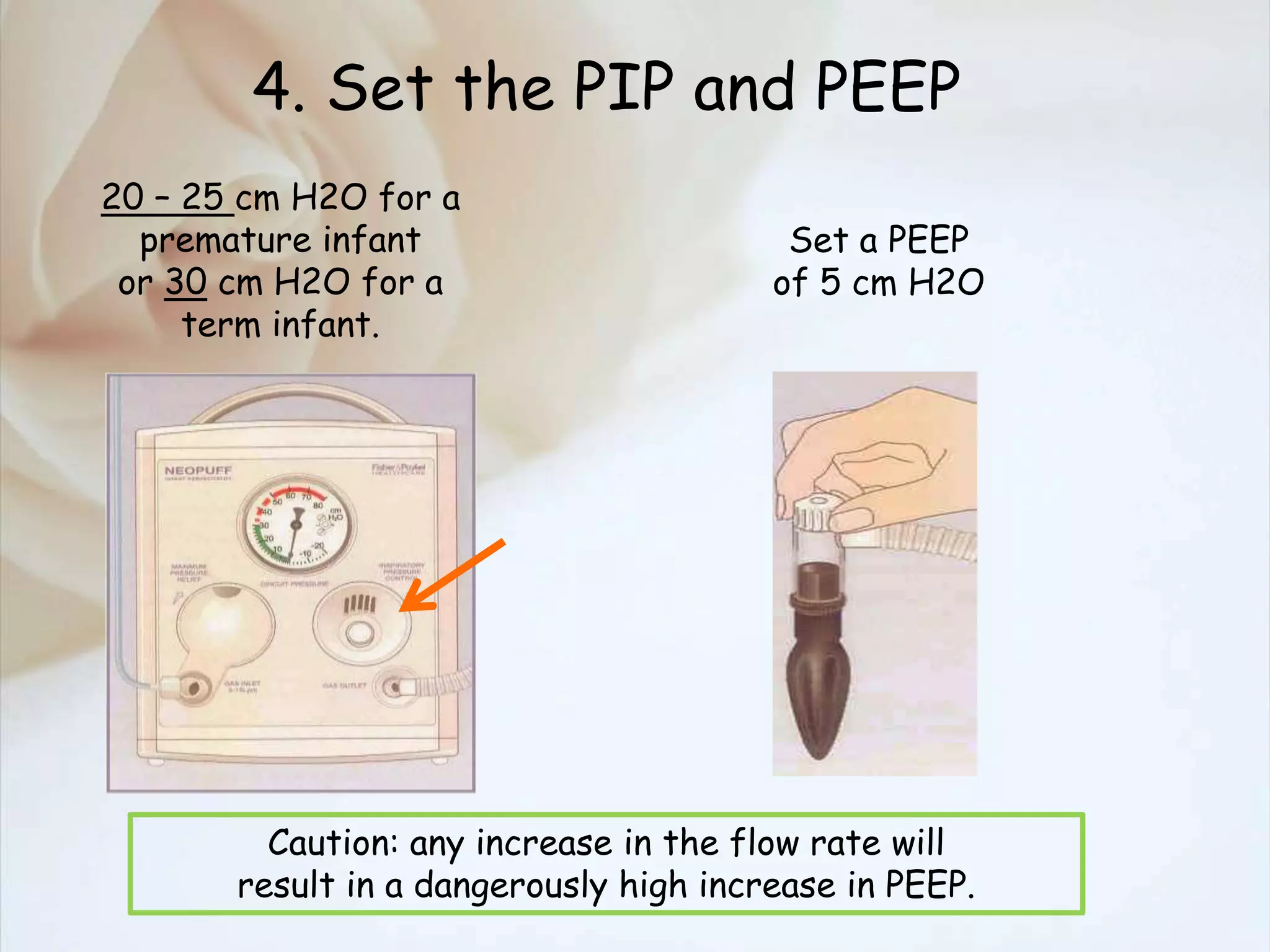
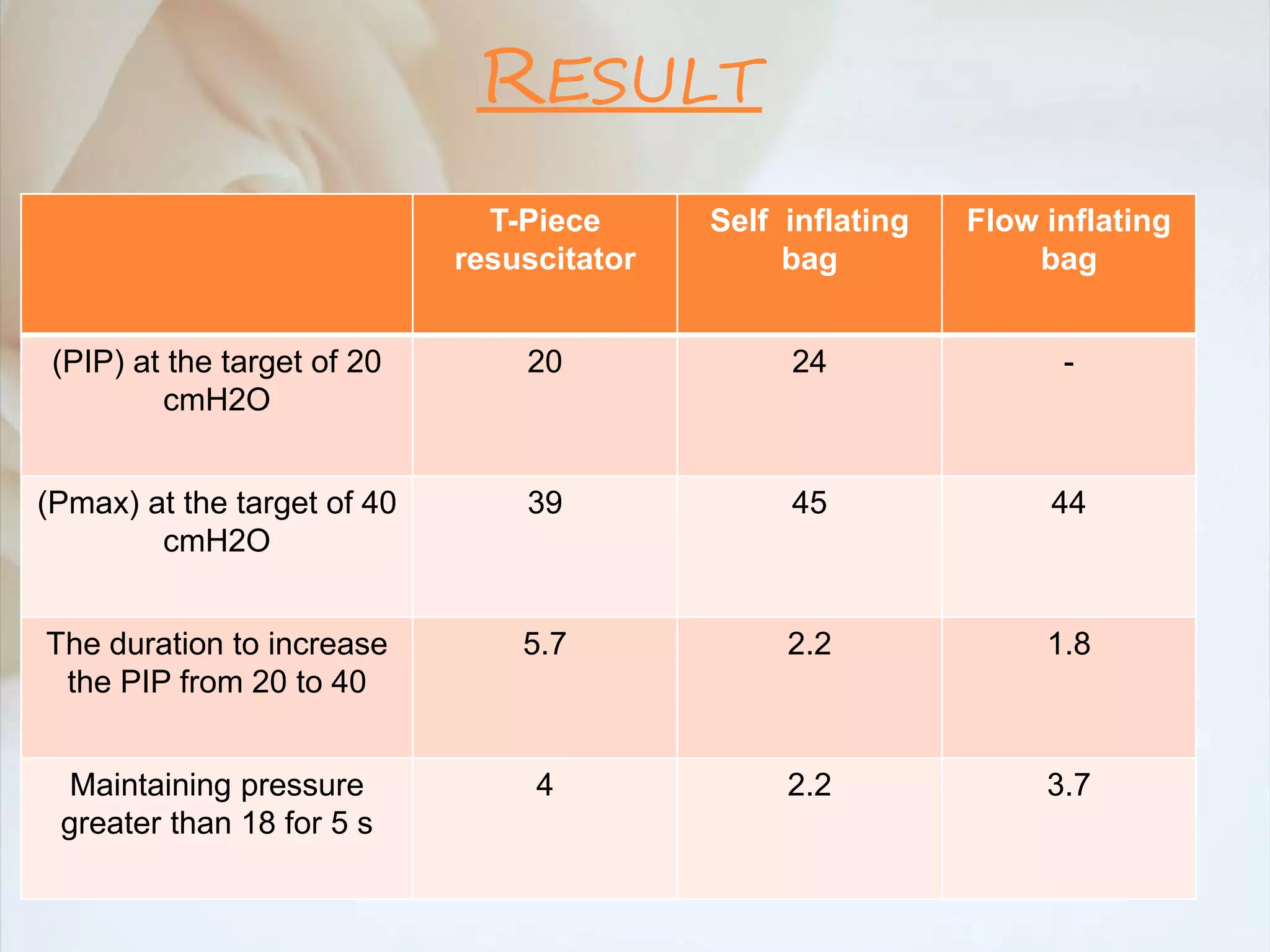
The document outlines the process and devices used for neonatal resuscitation, including self-inflating bags, flow inflating bags, and T-piece resuscitators, detailing their mechanisms, effectiveness, and usage protocols. It emphasizes the importance of proper technique in assessing ventilation effectiveness and discusses the results of studies comparing these devices. Safety limitations regarding flow rates and potential hazards from incorrect use are also highlighted.