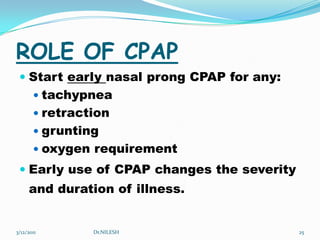
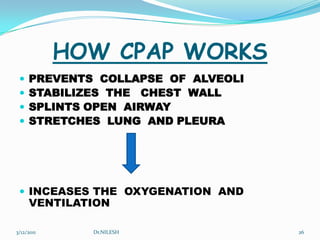
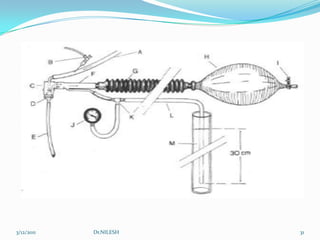
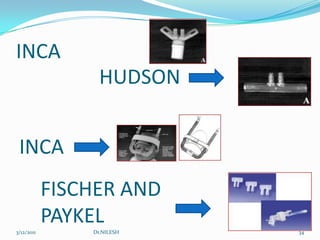
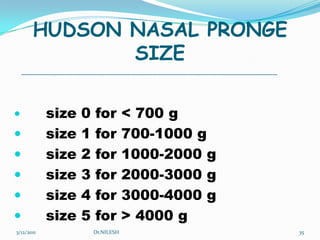
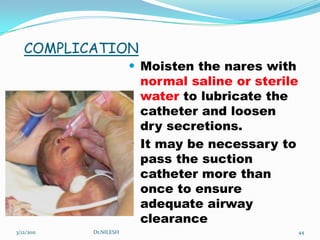
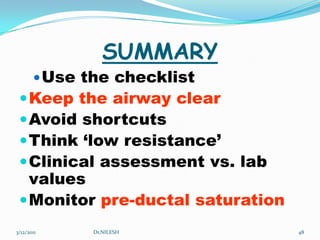
This document discusses ventilator settings and CPAP. It provides an overview of basics of ventilators and ventilator settings. CPAP is described as preventing alveolar collapse, stabilizing the chest wall, and splinting the airway open. Different types of CPAP generators and components are outlined. Bubble CPAP is discussed as a simple and cost effective method. Advantages, initiation, monitoring and complications of CPAP are summarized. Factors in determining ventilator settings and their effects are also reviewed.