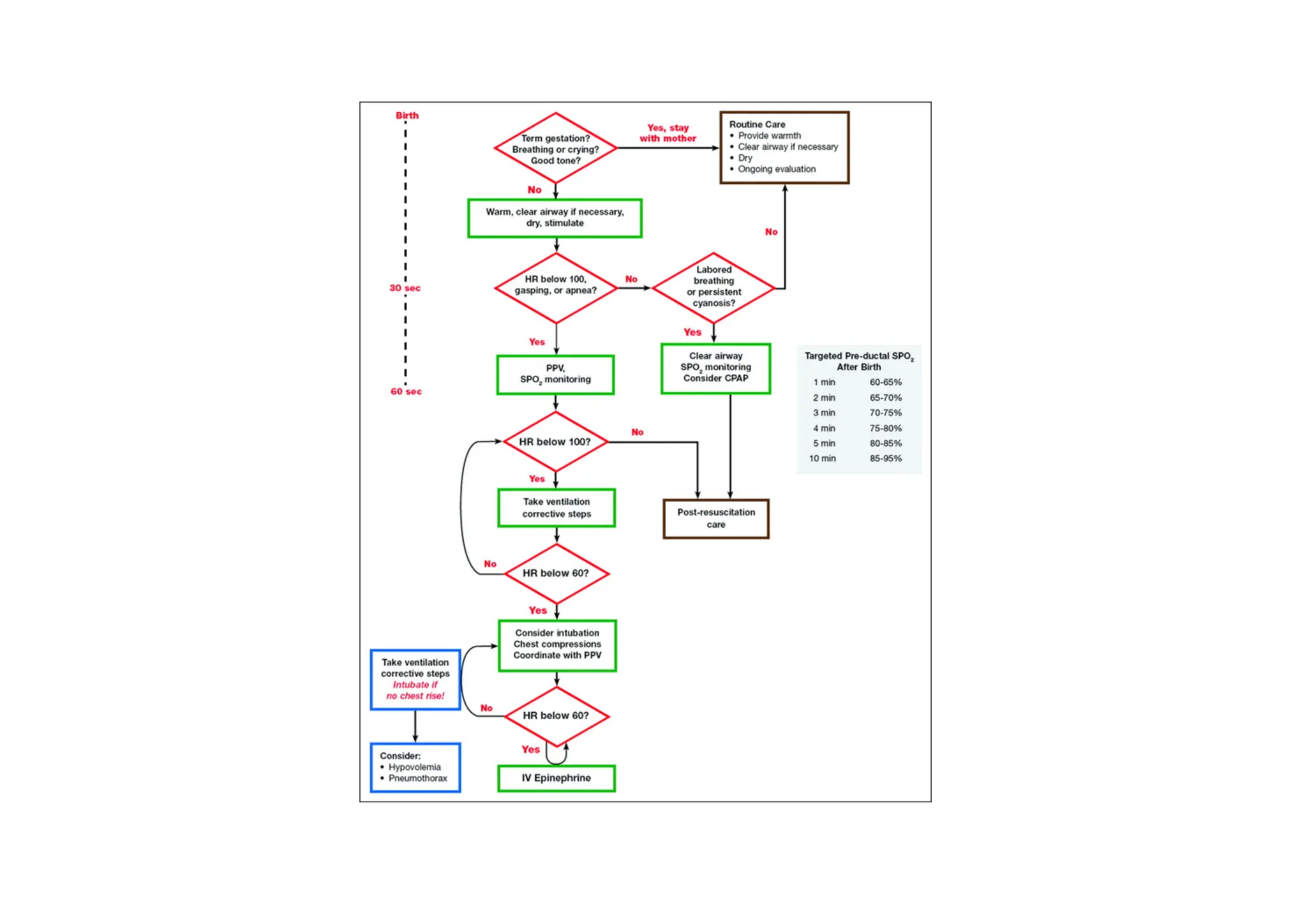
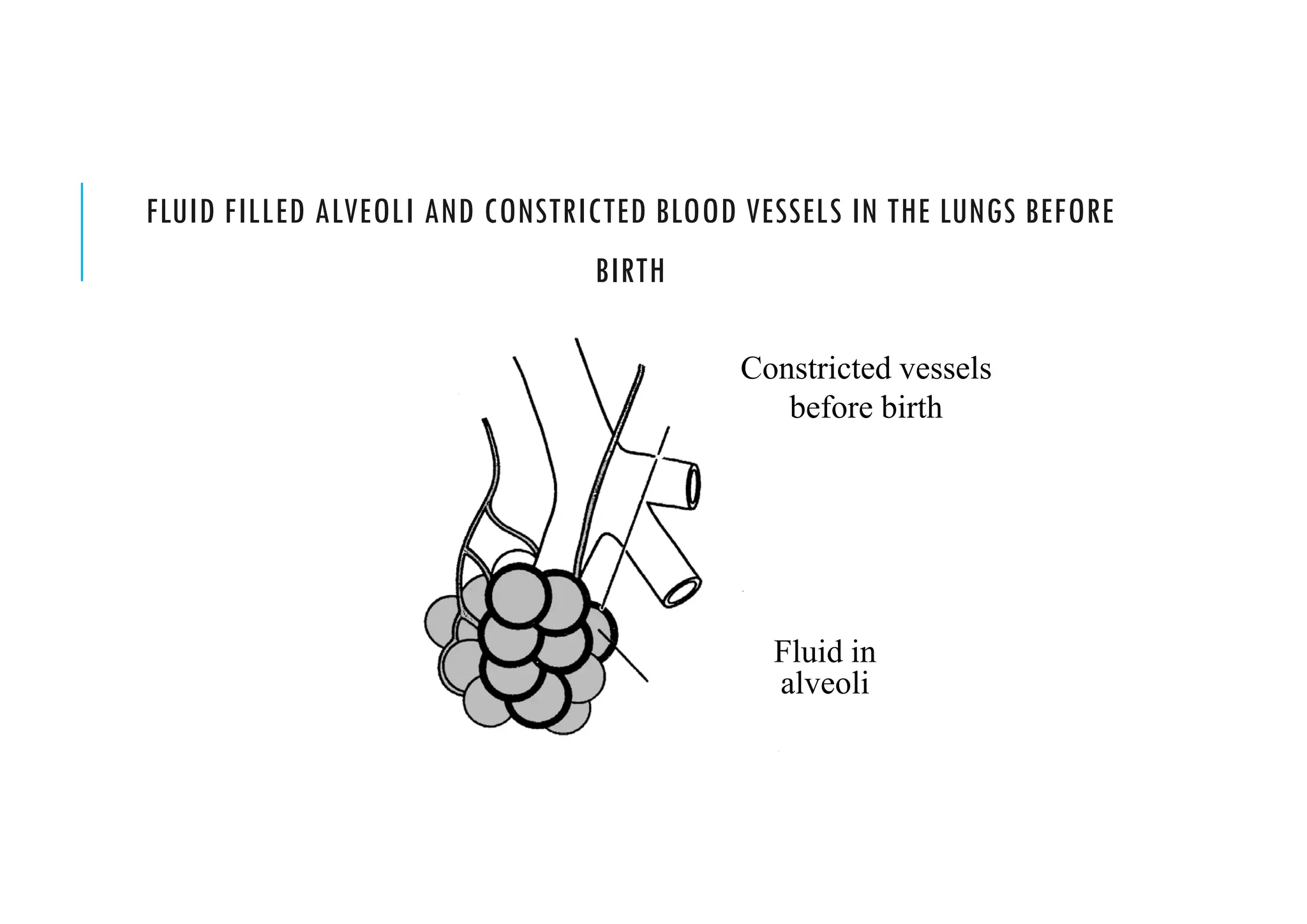
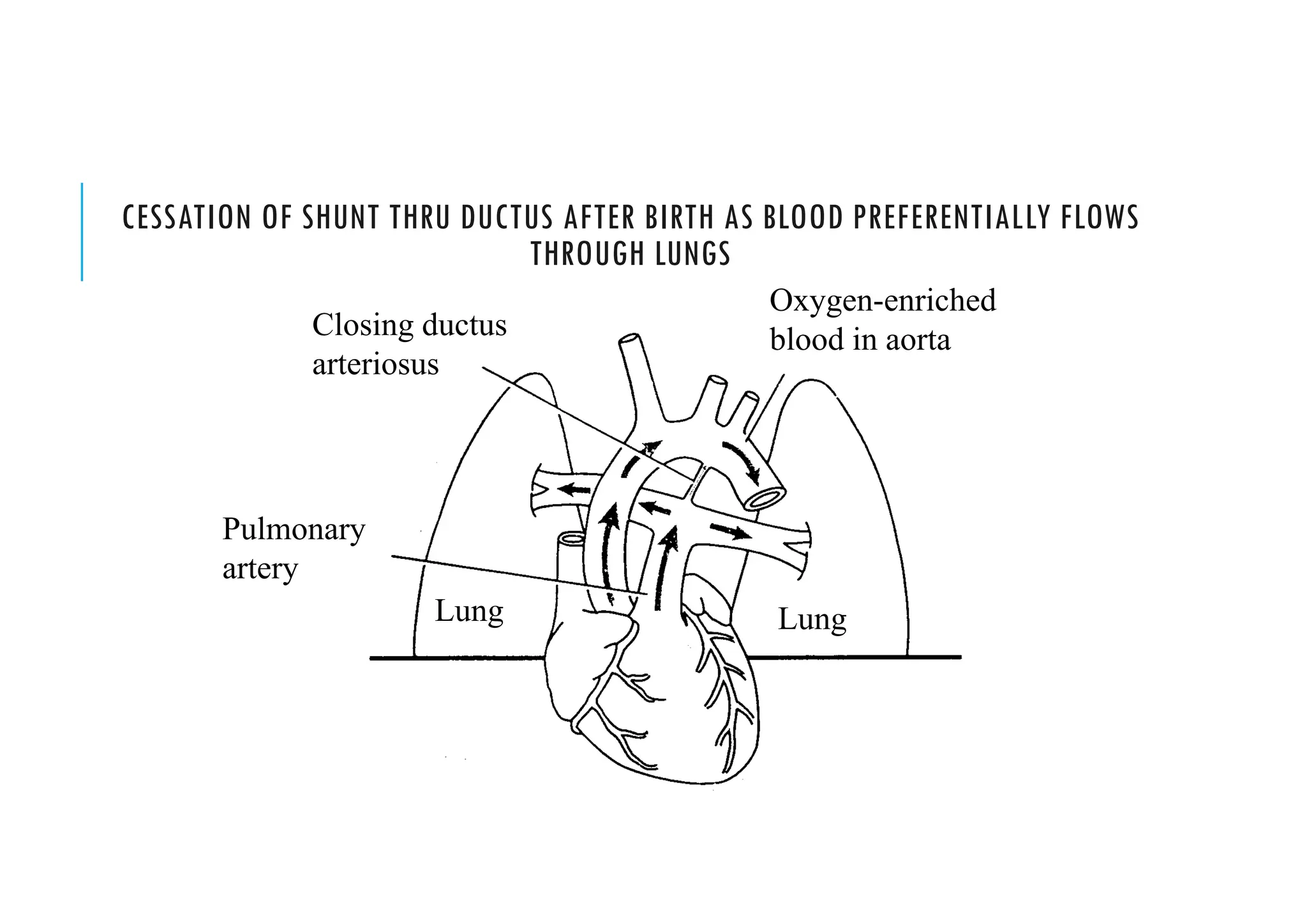
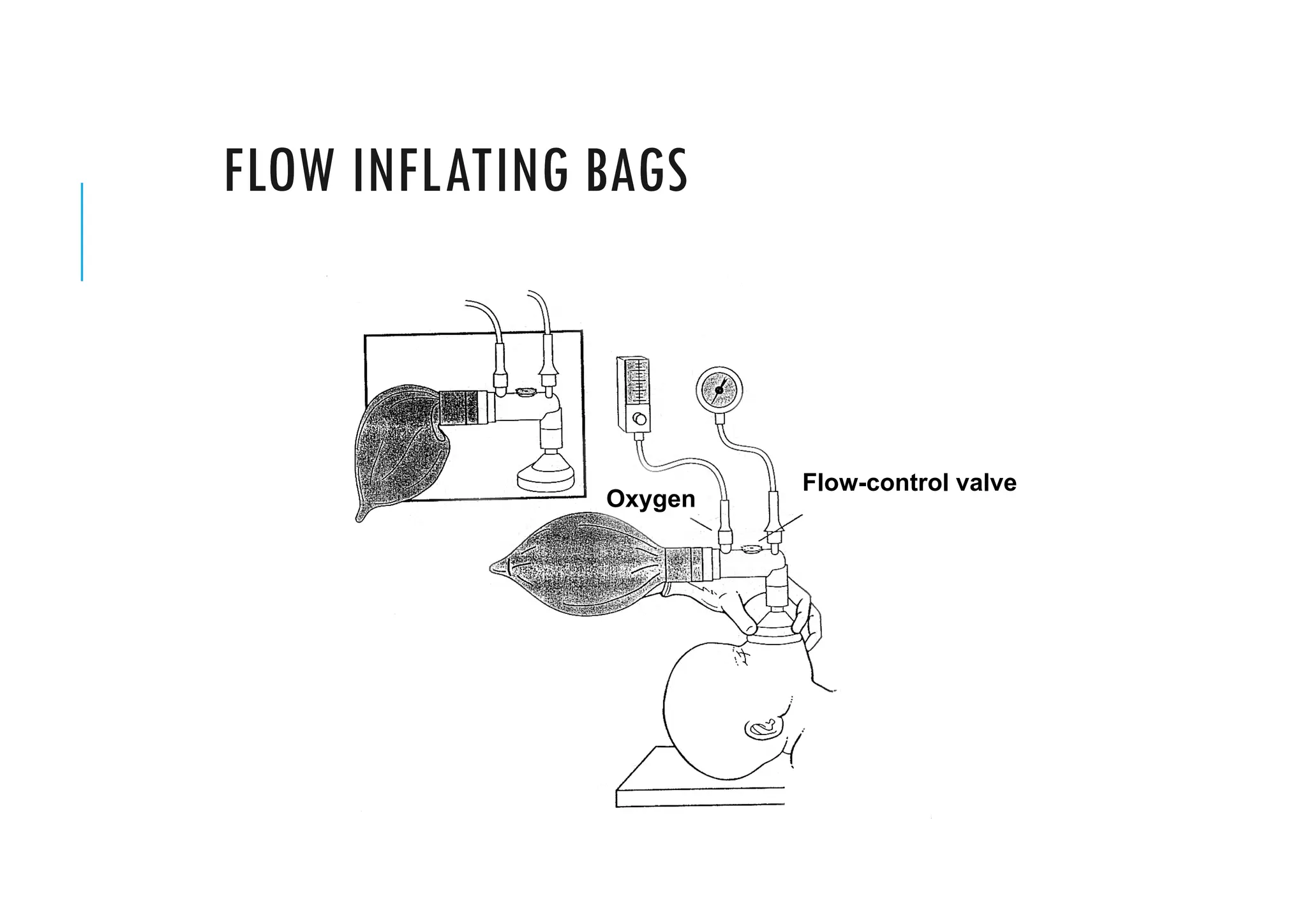
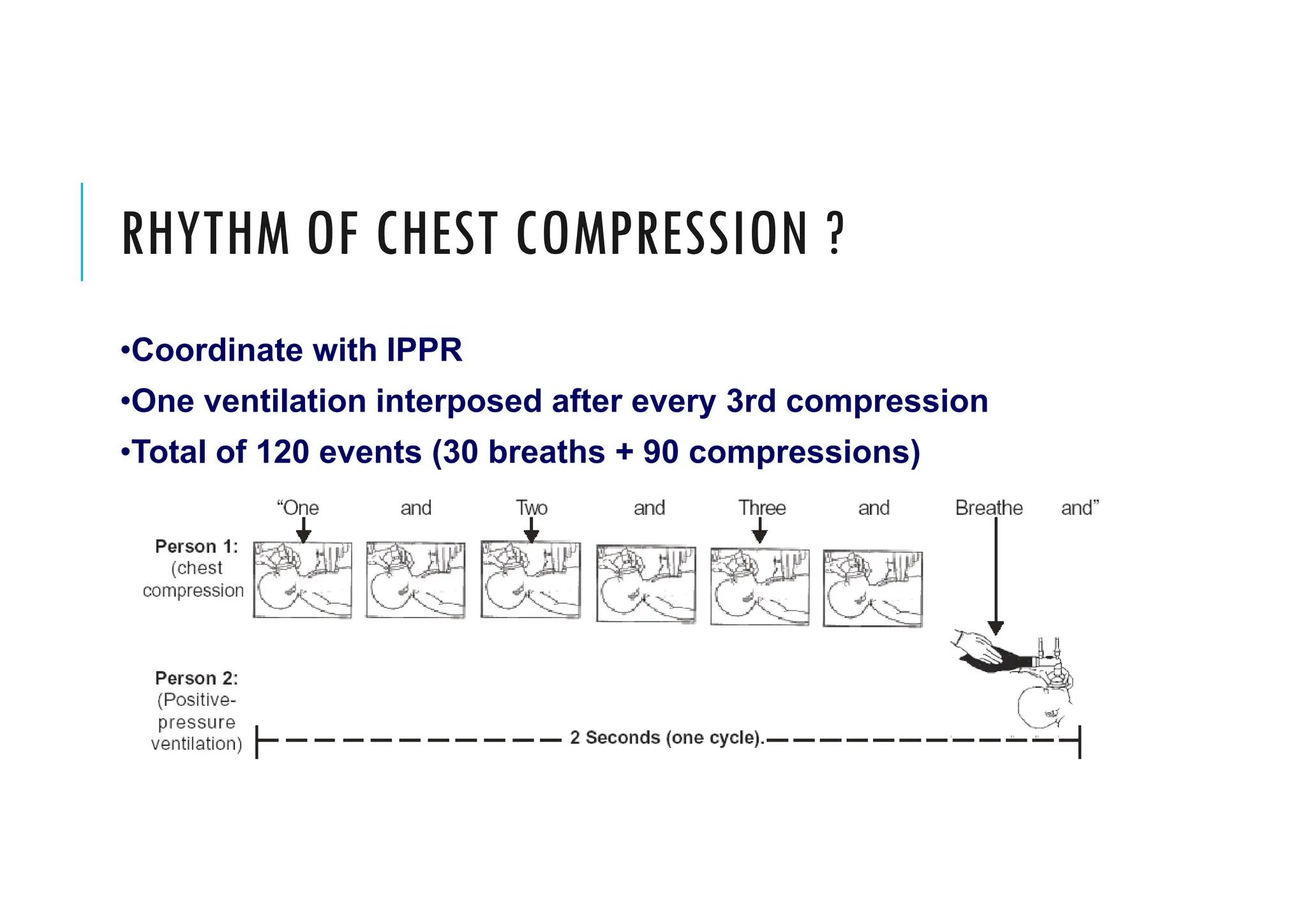
This document provides guidelines for neonatal resuscitation. It discusses the importance of resuscitation in improving outcomes for newborns, covering the ABCs which include clearing the airway, stimulating breathing, and assessing circulation. It describes the normal transition that occurs at birth and what can go wrong, such as inadequate breathing or blood flow issues. The key principles of anticipation and assessment of oxygen need are covered. The indications and techniques for positive pressure ventilation and chest compressions are outlined, as well as when medications may be required.