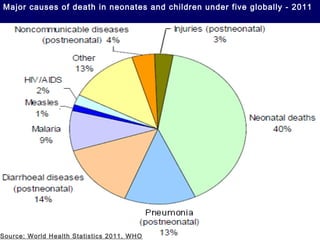
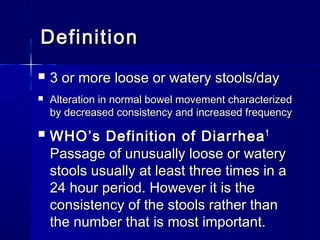
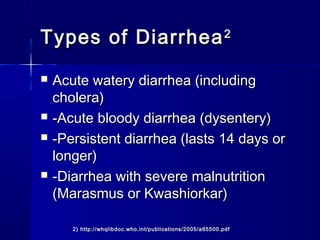
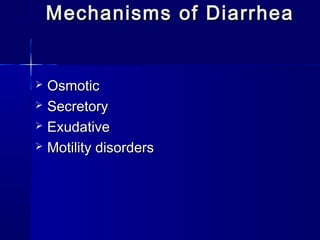
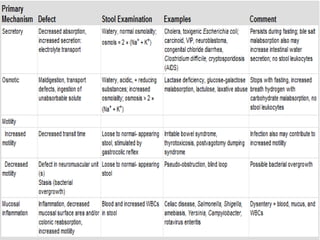
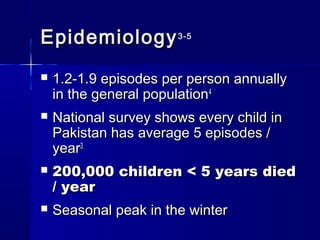
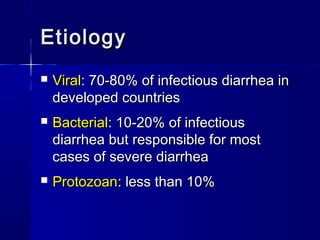
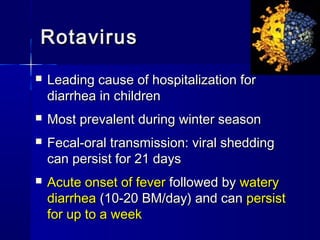
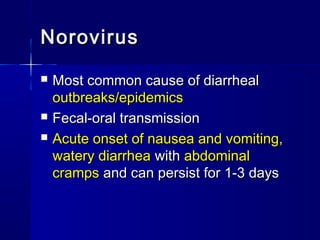
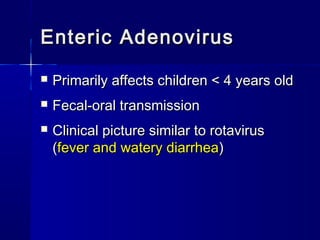
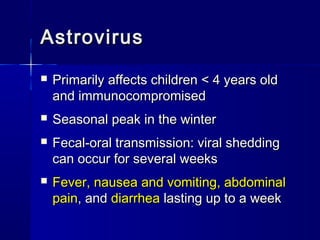
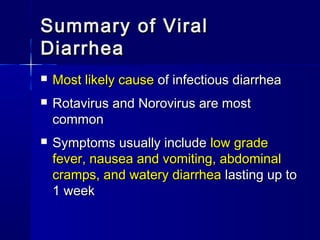
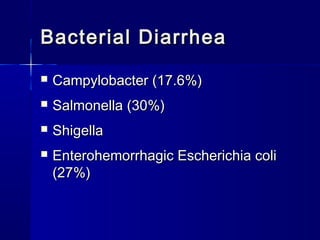
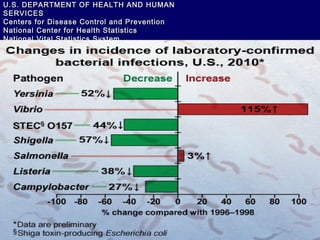
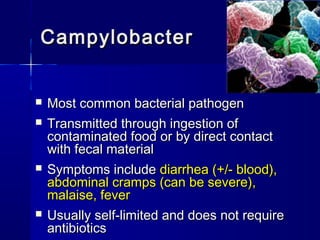
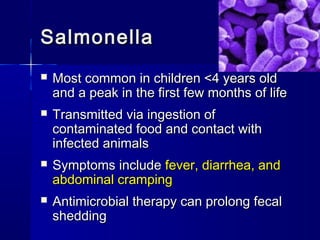
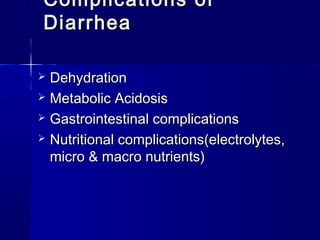
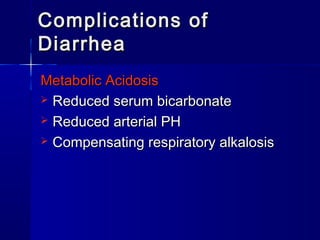
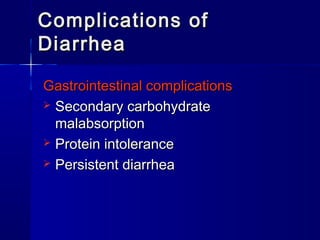
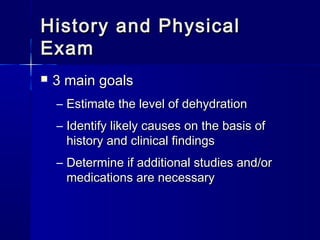
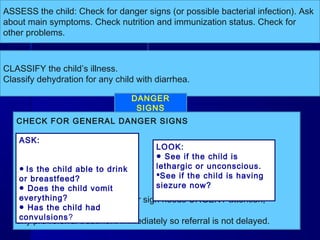
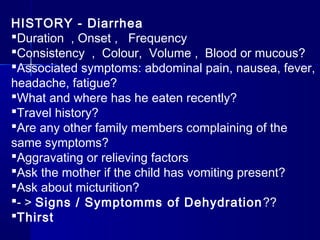
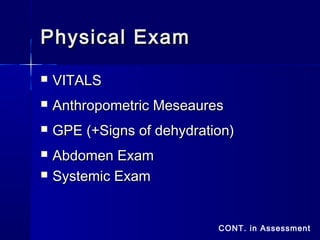
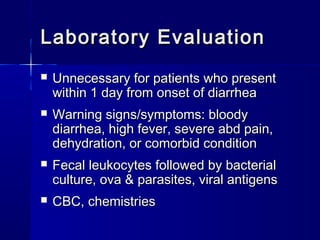
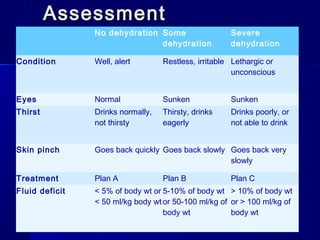
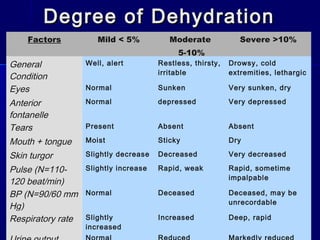
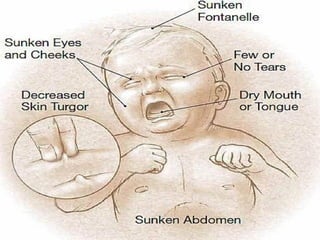
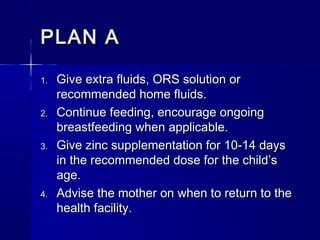
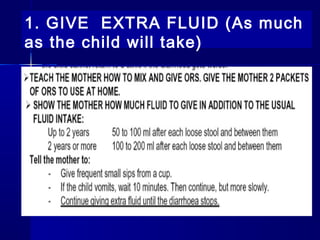
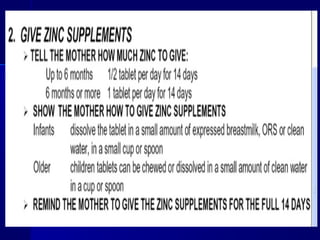
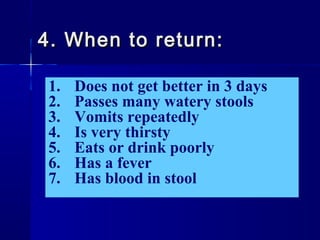
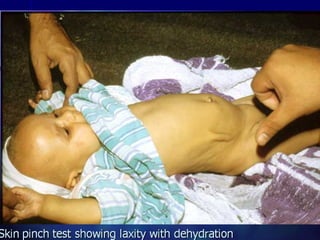
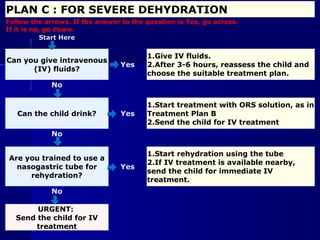
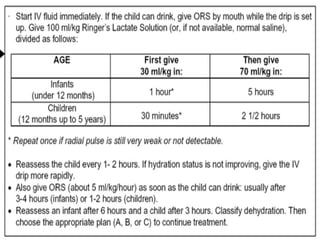
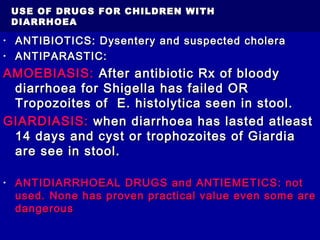
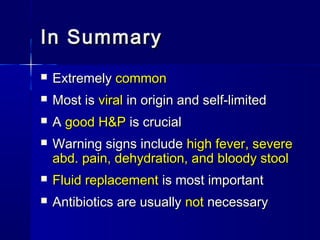
Diarrhea is the second leading cause of death in children worldwide. It can be caused by viruses like rotavirus and norovirus, bacteria such as campylobacter and salmonella, or parasites. Symptoms typically include fever, abdominal cramps, and watery diarrhea lasting up to one week. Complications may include dehydration, nutritional deficiencies, and persistent diarrhea. Proper diagnosis and treatment focuses on rehydration and identifying signs of dehydration or bacterial infection.