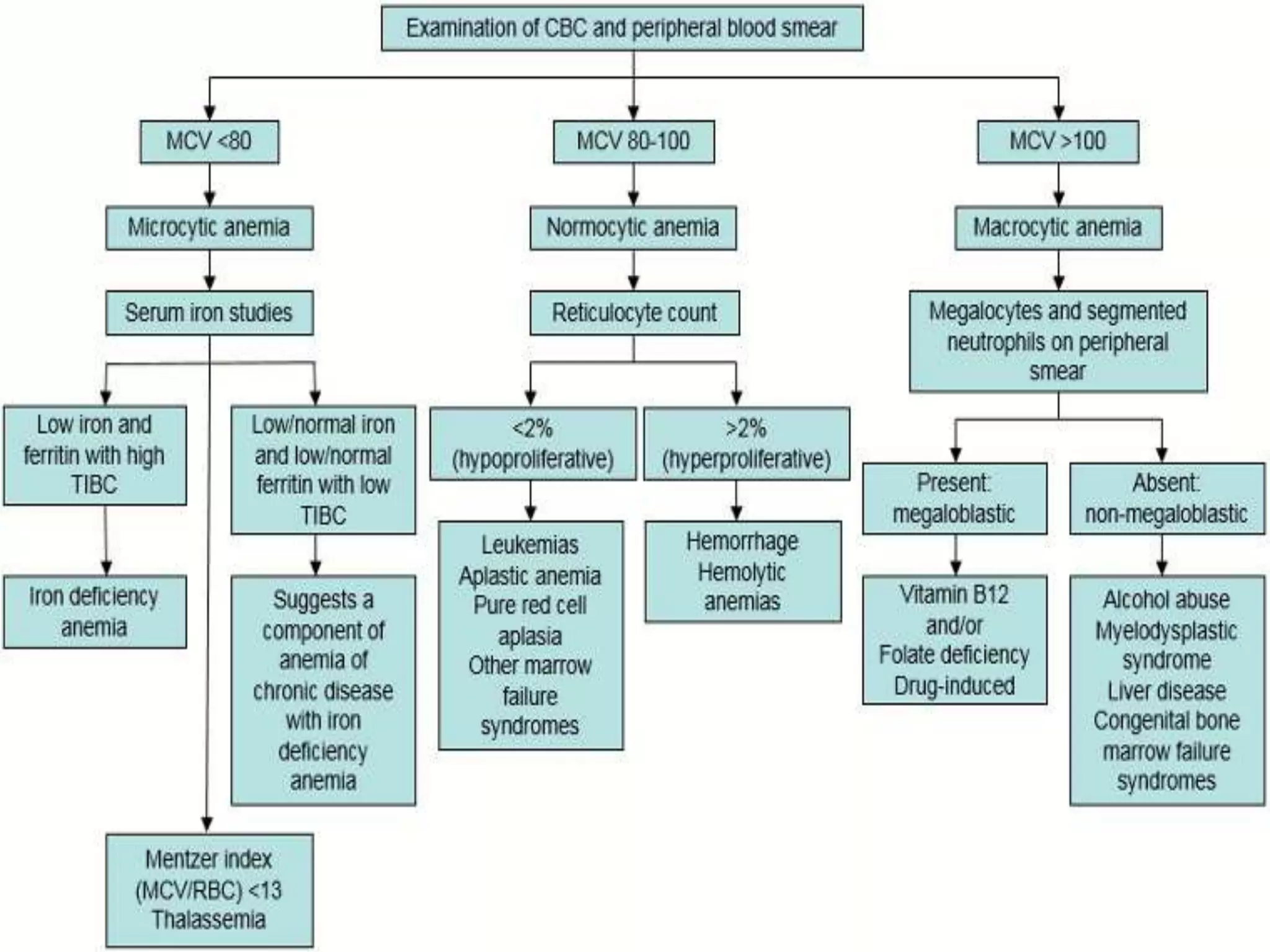
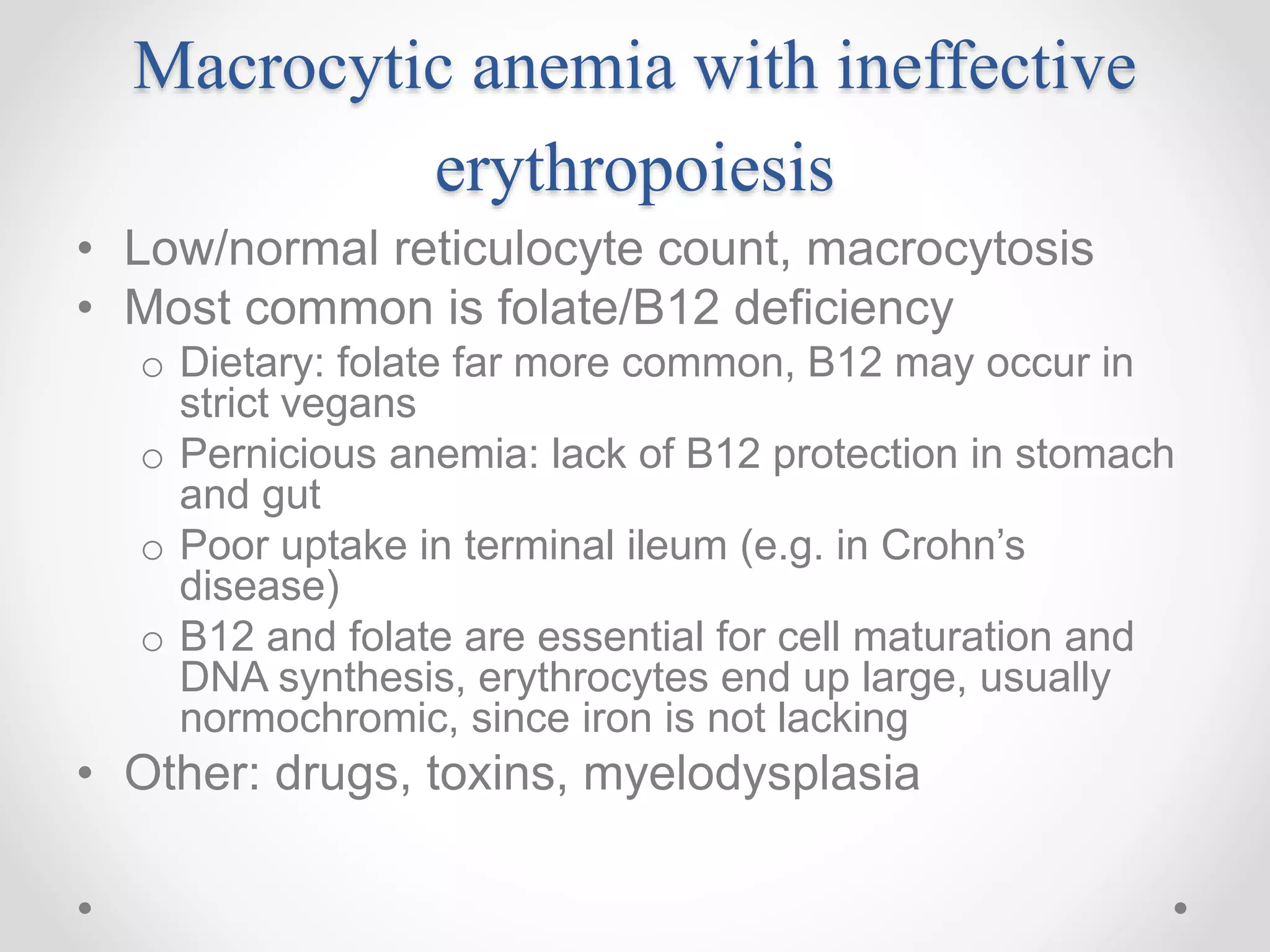
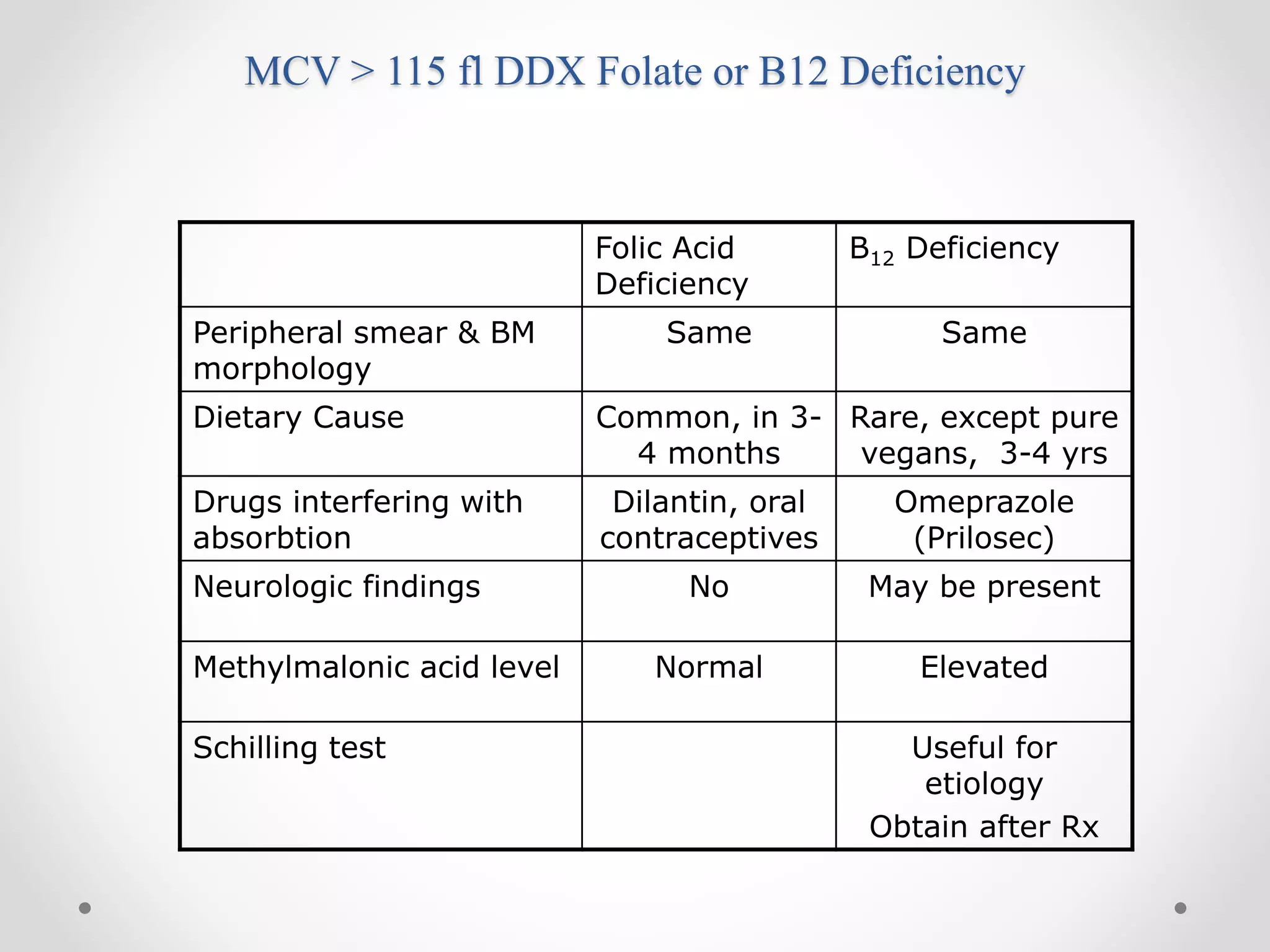
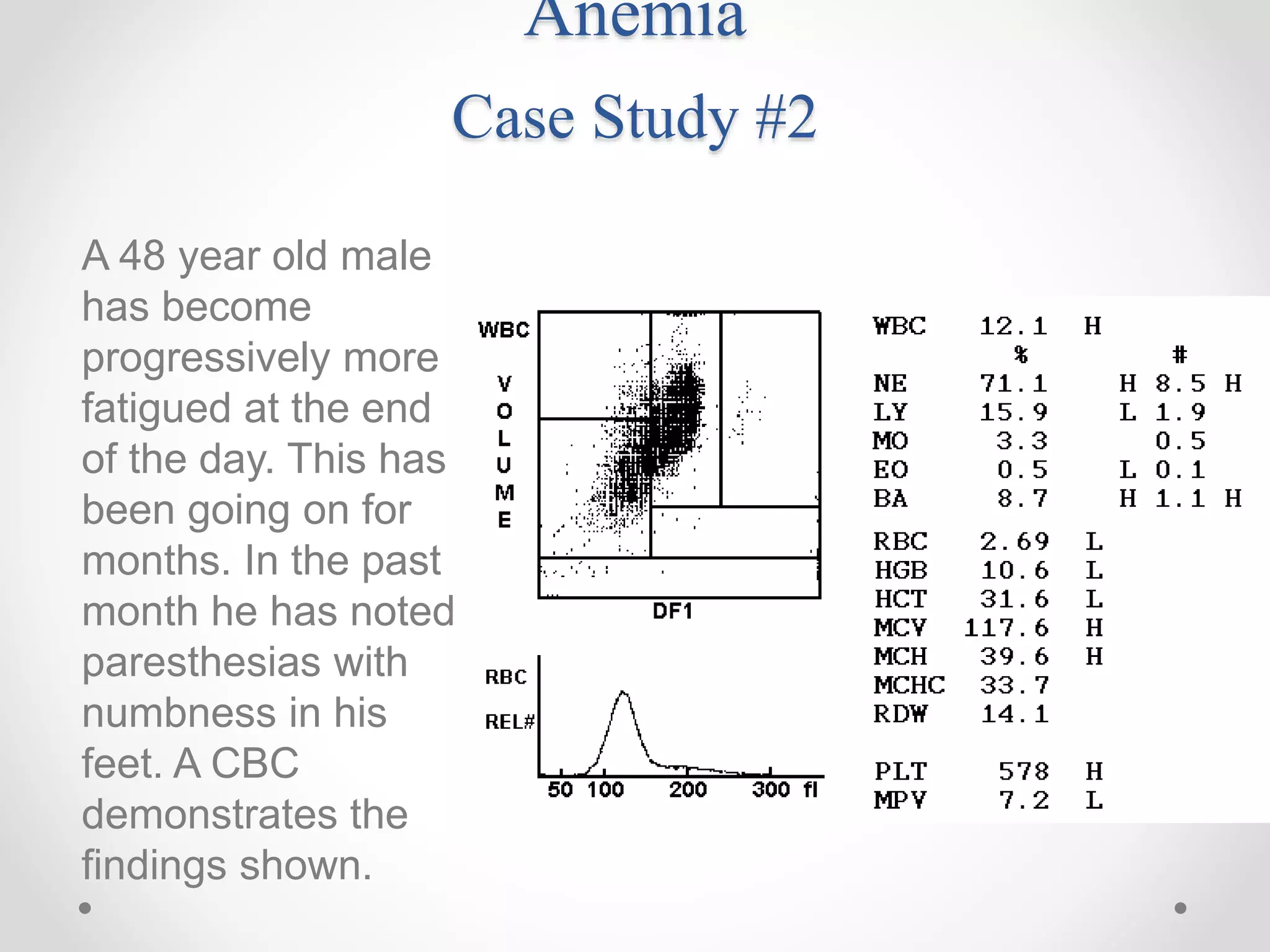
The diagnosis is vitamin B12 deficiency (pernicious anemia).
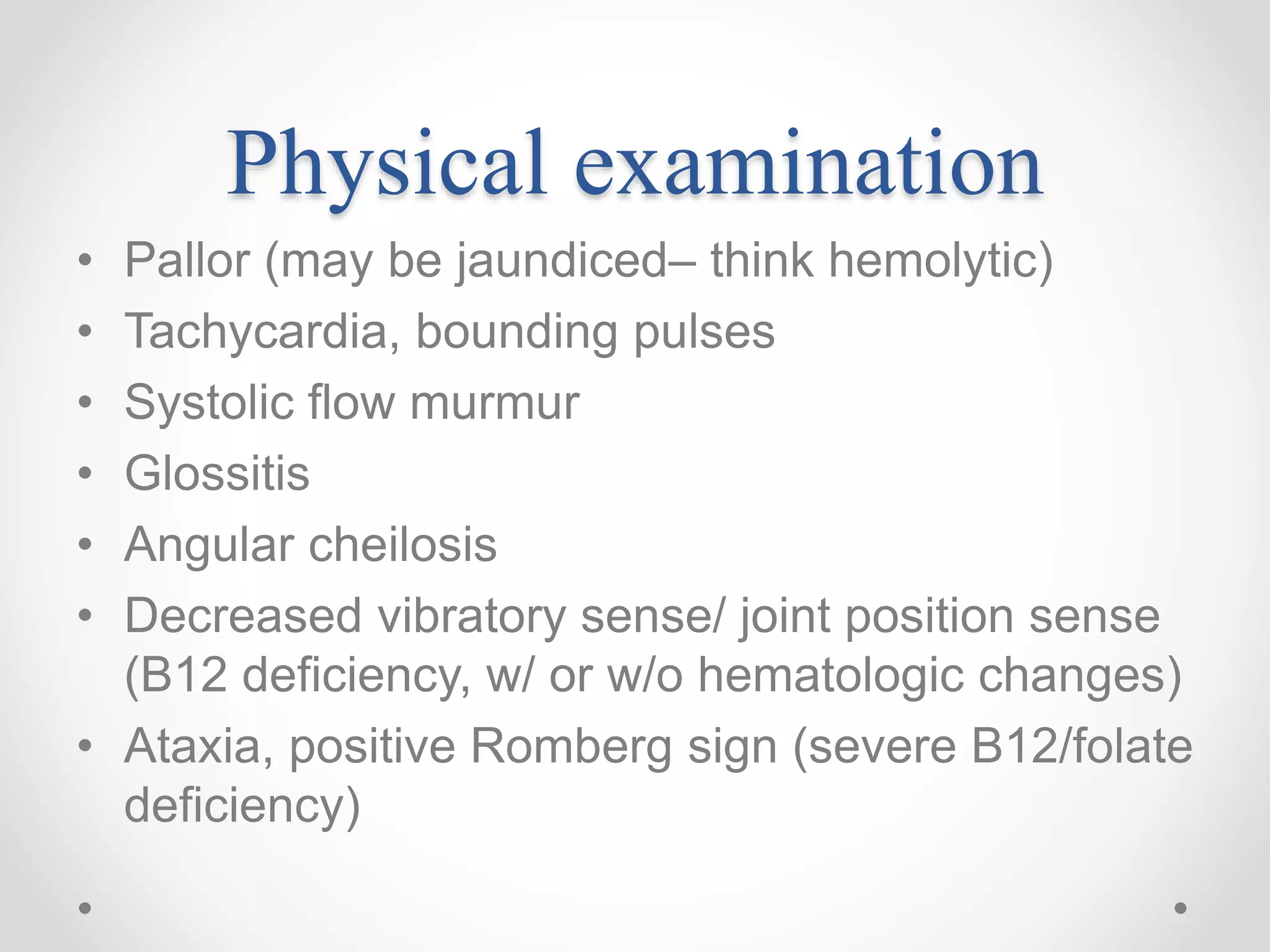
The neurologic findings can be explained by the fact that severe B12 deficiency can damage the dorsal and lateral columns of the spinal cord, leading to decreased vibratory sense, loss of position sense in the joints, and possibly ataxia. This is because B12 is essential for myelin formation and maintenance in the nervous system.
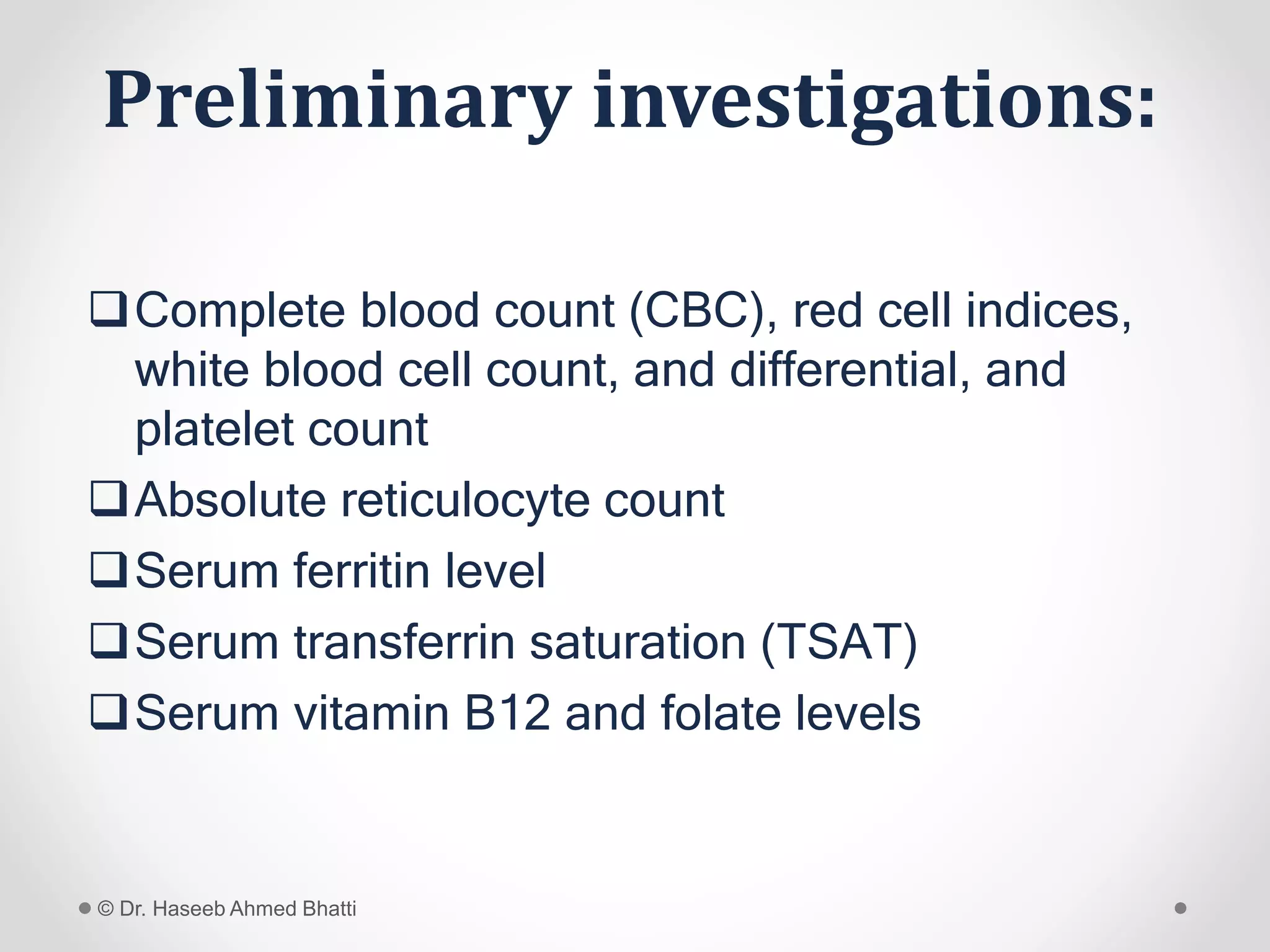
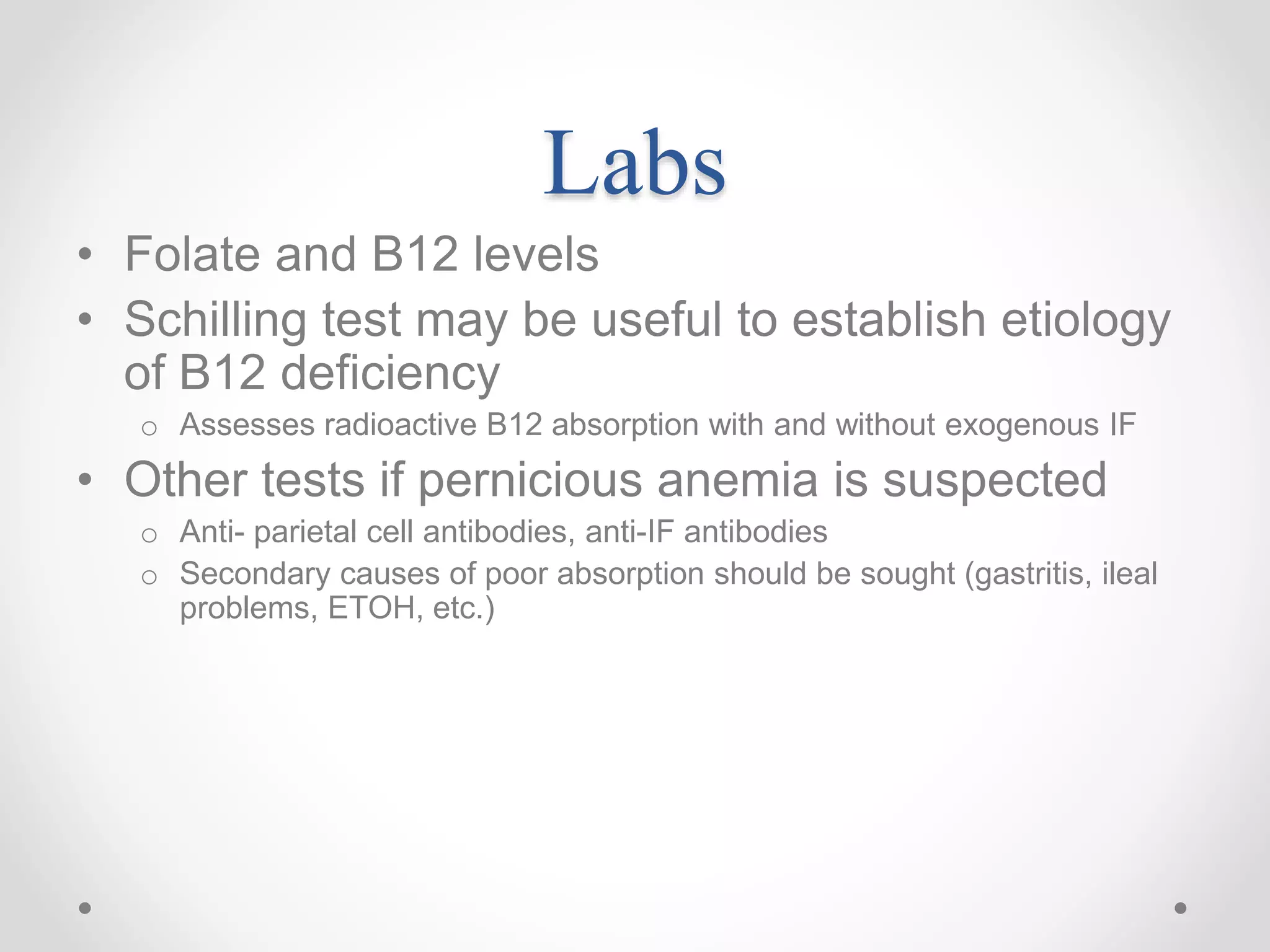
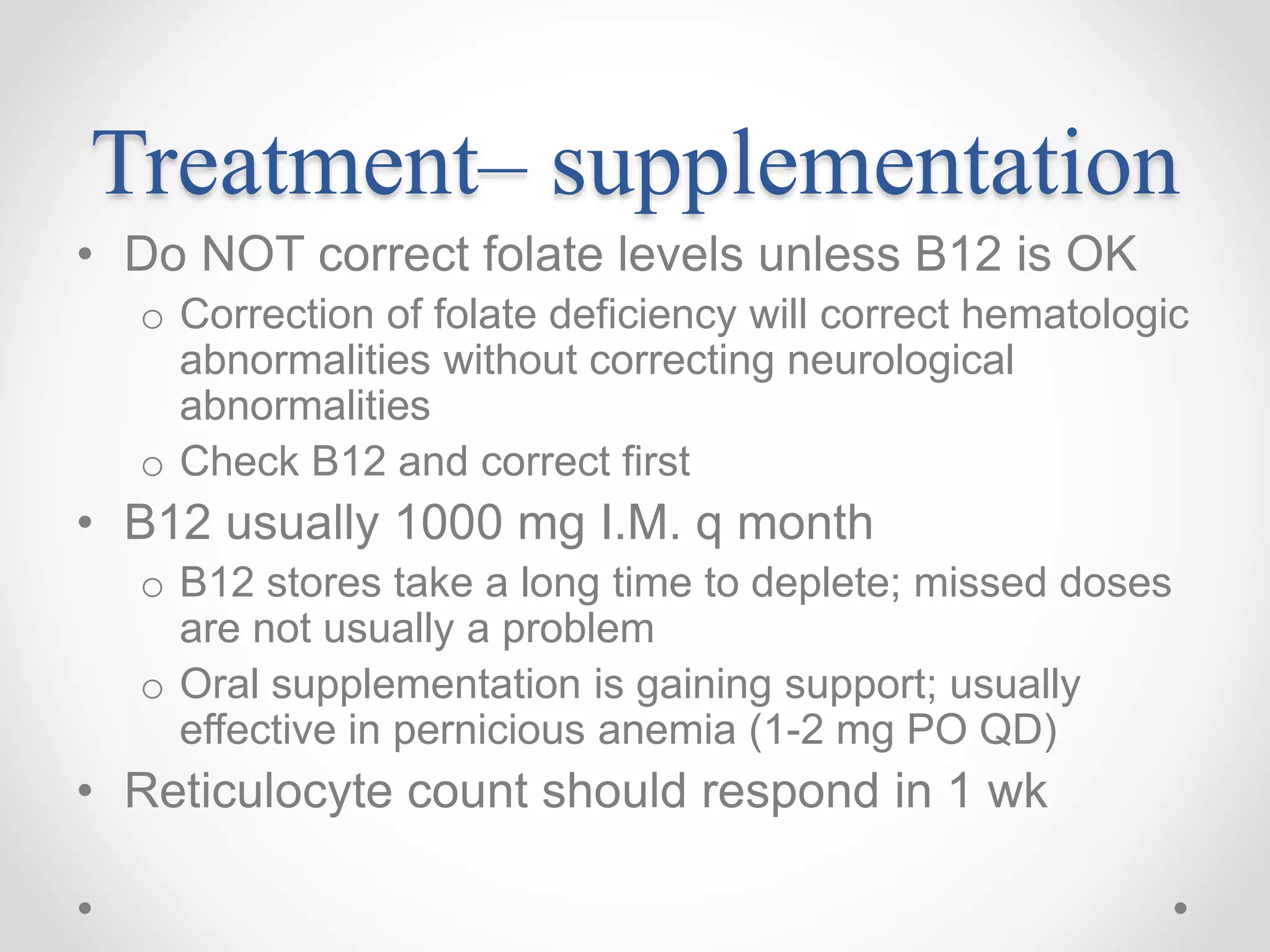
The next step would be to measure the patient's serum B12 level and consider treatment with parenteral B12 injections if deficient.