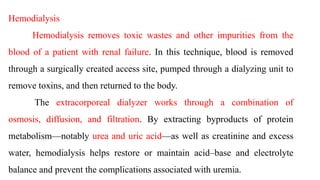
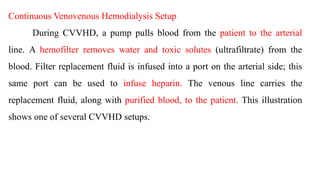
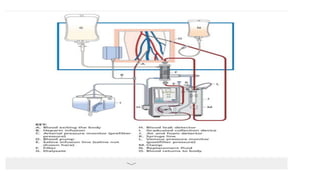
Continuous renal replacement therapy (CRRT) provides continuous dialysis treatment for patients with acute renal failure who cannot tolerate traditional intermittent hemodialysis. CRRT works around the clock to provide stable therapy without dangerous electrolyte and hemodynamic changes. There are various CRRT methods that differ in complexity, including continuous venovenous hemodialysis (CVVHD) where blood is pumped through a hemofilter to remove waste and fluids. CRRT requires vascular access via a catheter and uses pumps, hemofilters, replacement fluids, and dialysate to continuously clean and filter the blood. Nursing responsibilities for CRRT include monitoring vitals, equipment, lines, medications, schedules, and managing complications.