Here are potential responses to the questions:
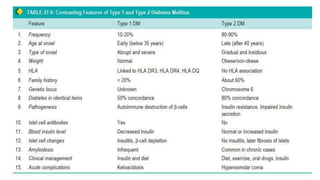
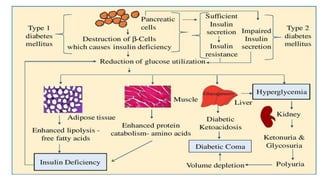
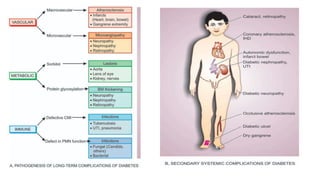
1. Diabetes mellitus is a chronic metabolic disorder characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Complications of diabetes include:
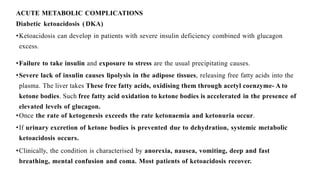
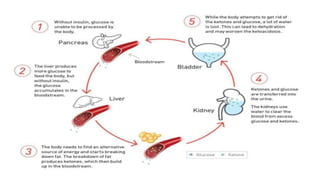
- Acute complications like diabetic ketoacidosis and hyperosmolar hyperglycemic state.
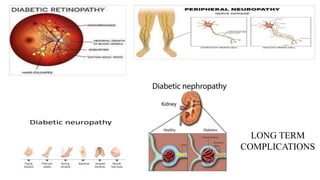
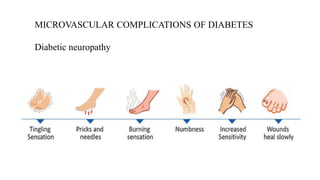
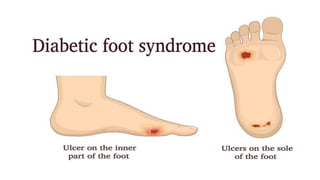
- Microvascular complications like diabetic retinopathy (leading to blindness), nephropathy (leading to renal failure) and neuropathy (causing pain and impaired healing).
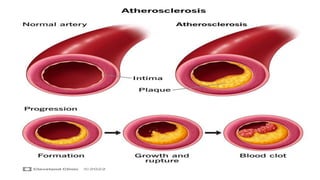
- Macrovascular complications like atherosclerosis leading to cardiovascular disease (heart attacks and strokes), peripheral vascular disease (leg pain and poor wound healing).
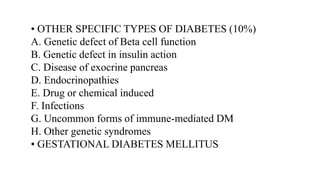
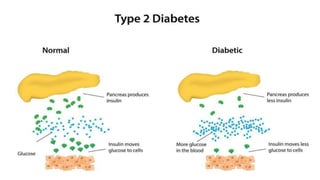
2. Diabetes is classified into Type 1 (caused by auto

![Classification and Etiology
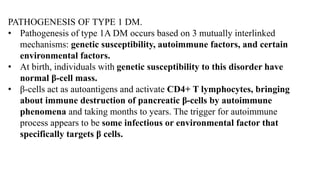
• TYPE 1 DIABETES MELLITUS (10%)
[Insulin-dependent, or juvenile-onset diabetes]
➢ TYPE 1A: Immune-Mediated
➢ Type 1B: Idiopathic
• Type 2 DIABETES MELLITUS (80%)
[Non-insulin dependent, maturity-onset diabetes]](https://image.slidesharecdn.com/diabetes-230623151936-0a9d8c94/85/Diabetes-pdf-4-320.jpg)