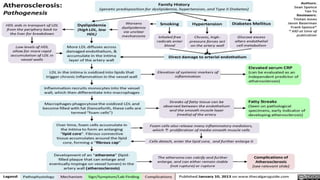
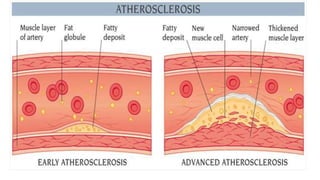
Atherosclerosis is a disease where plaque builds up in the arteries. Over time, the plaque hardens and narrows the arteries, limiting blood flow. Risk factors include age, family history, smoking, high blood pressure, high cholesterol, diabetes, and obesity. Complications arise when blood flow is reduced to organs like the heart, brain, kidneys, and limbs, potentially causing heart attacks, strokes, chronic kidney disease, or poor circulation. Treatment focuses on lifestyle changes and medications to control risk factors and symptoms.