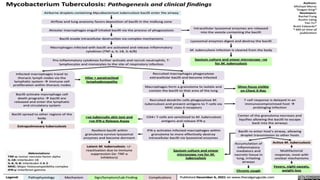
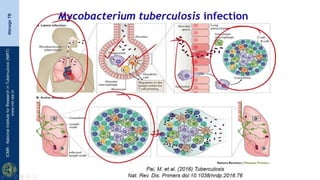
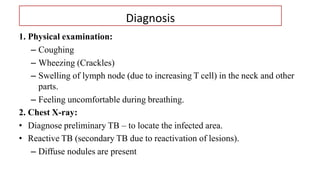
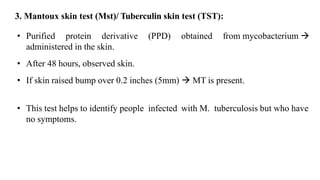
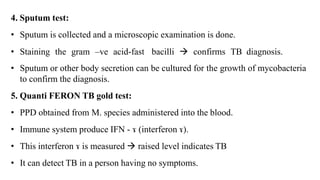
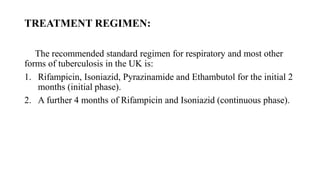
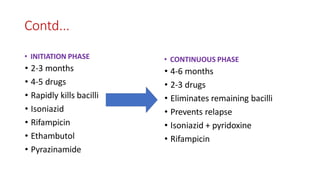
Tuberculosis (TB) is a chronic bacterial infection caused by Mycobacterium tuberculosis that typically forms granulomas in the lungs. It is treatable with a combination of anti-TB drugs over a 6-12 month period to kill both actively replicating and dormant bacilli. Diagnosis involves physical exam, chest x-ray, tuberculin skin test, and sputum culture. Risk factors include HIV infection, poverty, and crowded living conditions.