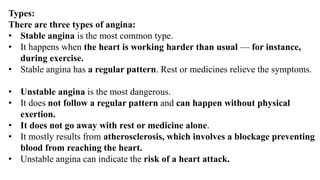
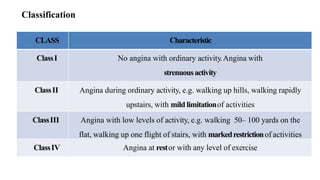
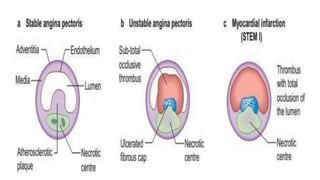
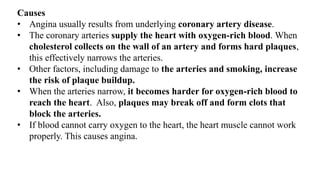
Ischaemic heart disease is caused by an imbalance between the heart's supply and demand for oxygenated blood, usually due to atherosclerosis narrowing the coronary arteries. The main symptoms are chest pain or discomfort known as angina. There are different types of angina that vary based on their triggers and patterns. Diagnosis involves tests like ECG, echocardiogram, stress tests and angiography. Treatment options include medications to reduce demands on the heart like nitrates, beta-blockers, and calcium channel blockers, as well as interventions like angioplasty, stents and bypass surgery.