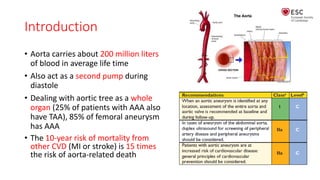
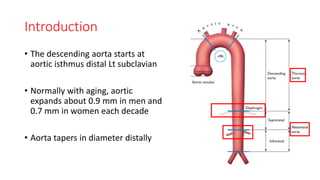
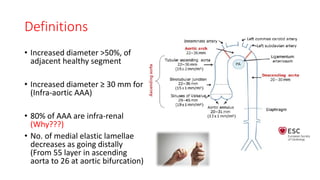
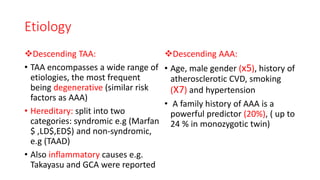
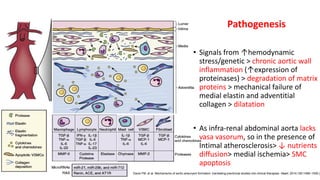
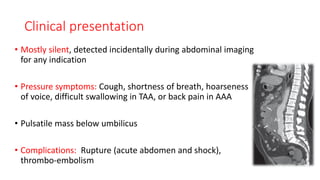
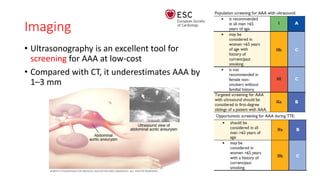
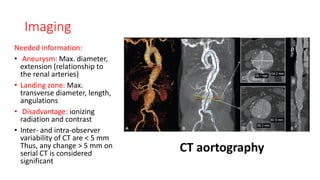
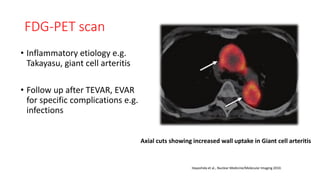
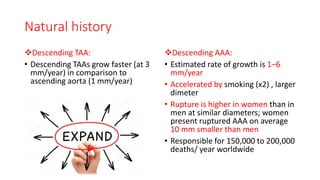
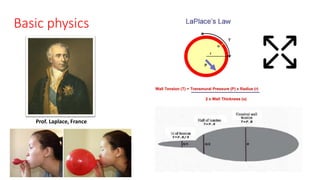
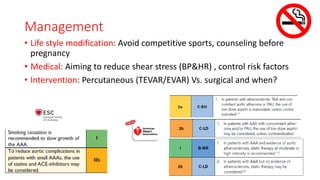
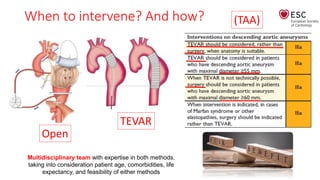
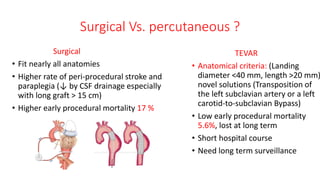
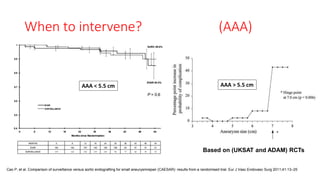
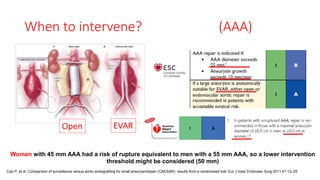
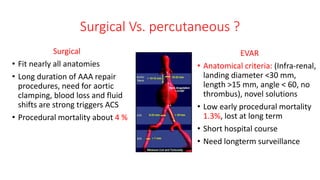
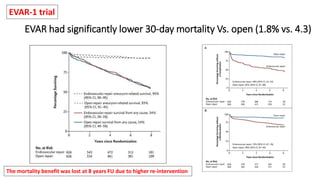
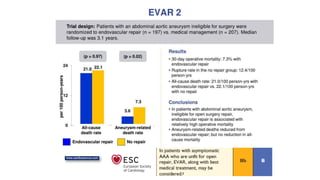
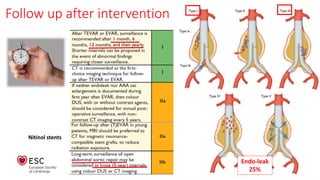
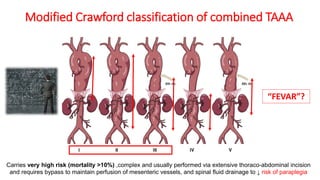
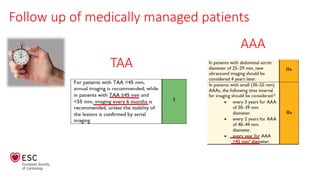
This document discusses descending aortic aneurysms, including their etiology, diagnosis, treatment options, and follow up. It notes that descending aortic aneurysms can be either true or false aneurysms. True aneurysms are usually degenerative in nature and share risk factors with abdominal aortic aneurysms like age, male sex, smoking, and hypertension. Imaging like CT or MRI is used to diagnose and monitor aneurysm size. Treatment depends on aneurysm size and anatomy, and may involve open surgical repair or endovascular stent grafting. Follow up care involves monitoring repaired aneurysms for complications like endoleaks. The overall goals are to control risk factors, intervene when aneurysms reach a certain size threshold based on guidelines, and