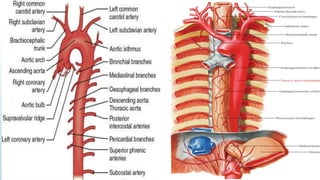
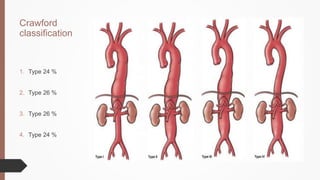
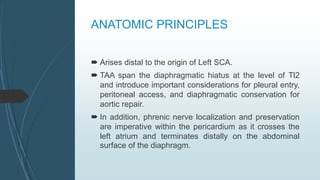
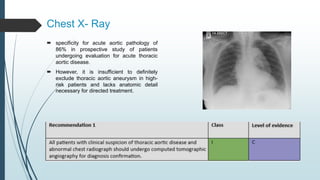
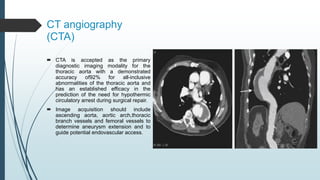
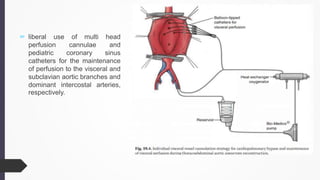
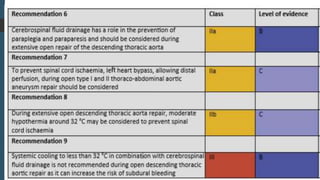
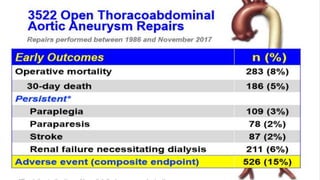
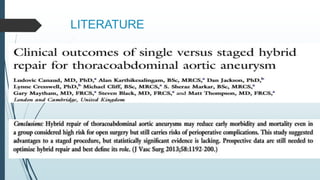
The document discusses the management of thoracoabdominal aortic aneurysms, detailing anatomical considerations, imaging modalities, and treatment options such as medical therapy, endovascular repair, and surgical techniques. It emphasizes critical factors in preventing spinal cord injury during procedures, including maintaining blood supply, careful pre-operative planning, and various protective strategies. The recommendations include patient monitoring, imaging selection based on individual needs, and techniques for minimizing post-operative complications.