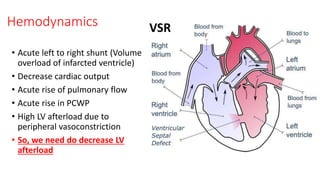
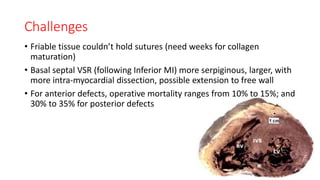
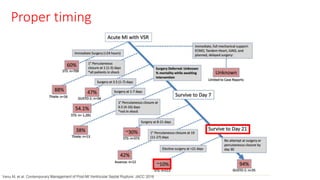
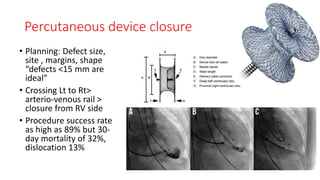
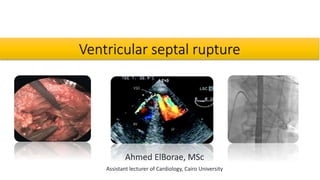
Ventricular septal rupture (VSR) is a devastating complication following myocardial infarction. It occurs in 0.17-0.31% of cases post-primary PCI, usually 2-8 days post-MI. Risk factors include older age, female sex, late presentation, extensive MI, hypertension, and lytic therapy. Diagnosis involves acute deterioration, auscultation findings, echocardiogram, and CT scan. Management uses a hybrid approach of primary PCI of the culprit vessel followed by transient mechanical support like IABP, then definitive surgical or percutaneous repair. Without treatment, mortality is over 90% at 1 year. Challenges include friable tissue that cannot hold sutures early on and
![Introduction
• (VSR) remains a devastating complication following MI
• Incidence: Decreased from 1-3% “pre-reperfusion era” to “0.17-0.31%” post
1ry PCI, [RCA in 46%- LAD in 42%]
• Onset: Average 2-8 days post MI, yet might occur earlier
• Risk factors: Old age-female-Late presentation-extensive MI HTN-Lytic therapy
• Diagnosis: Acute deterioration-auscultation “V.important”- Echo- MSCT
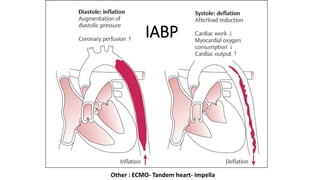
• Management: Hybrid approach (1ry PTCA of culprit- transient mechanical
support e.g. IABP) then definitive (Surgical or percutaneous)
• Prognosis: Without treatment > 90% mortality at 1 year
Venu M, et al. Contemporary Management of Post-MI Ventricular Septal Rupture. JACC 2018](https://image.slidesharecdn.com/vsr-220405155115/85/Ventricular-septal-rupture-pptx-2-320.jpg)