This document provides guidance on preparing for the European Exam in Core Cardiology (EECC). It outlines the exam format, resources for preparation, and topics covered. The key points are:
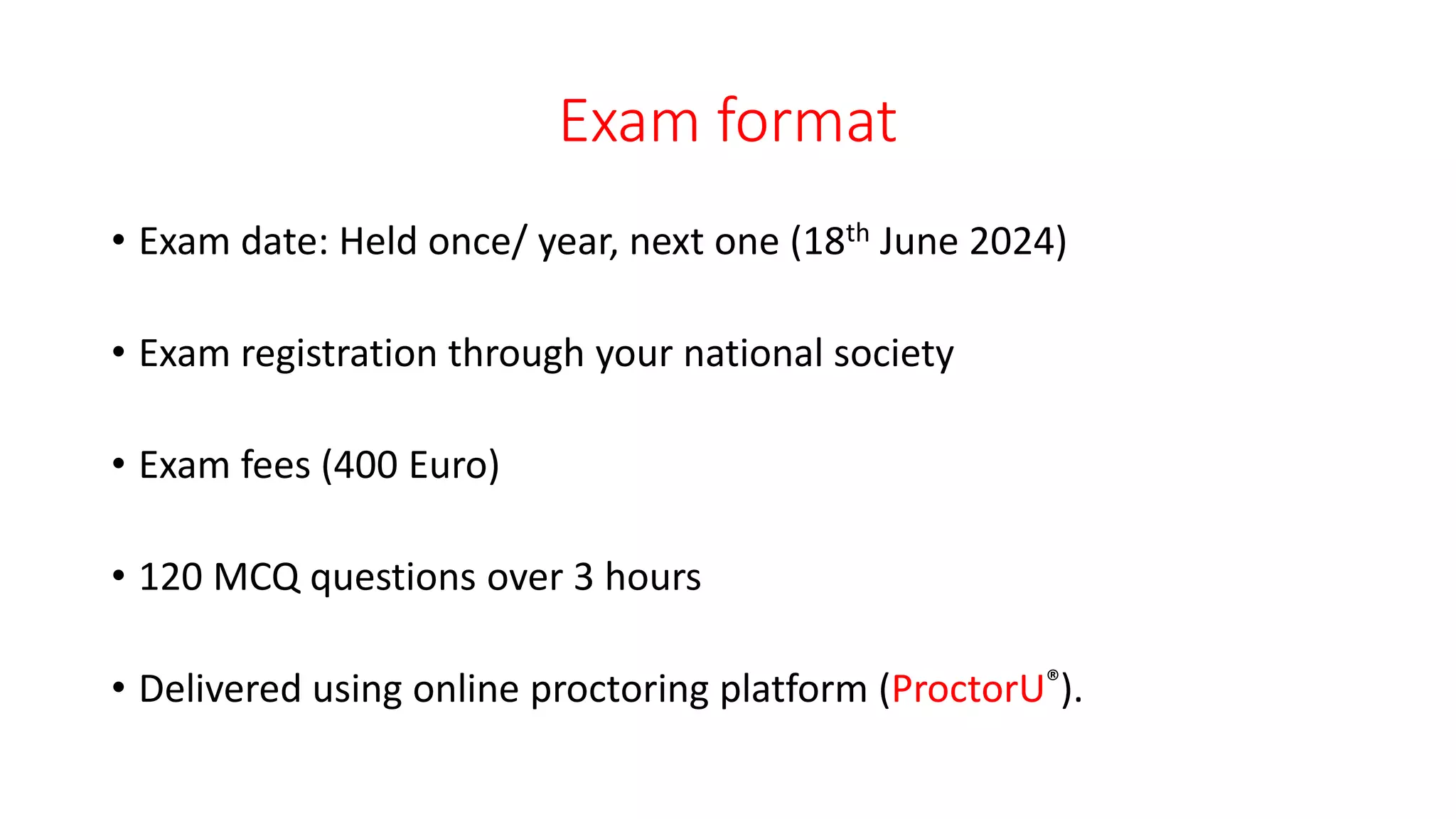
- The exam takes place once per year, with the next one in June 2024. It is 3 hours long and contains 120 multiple choice questions.
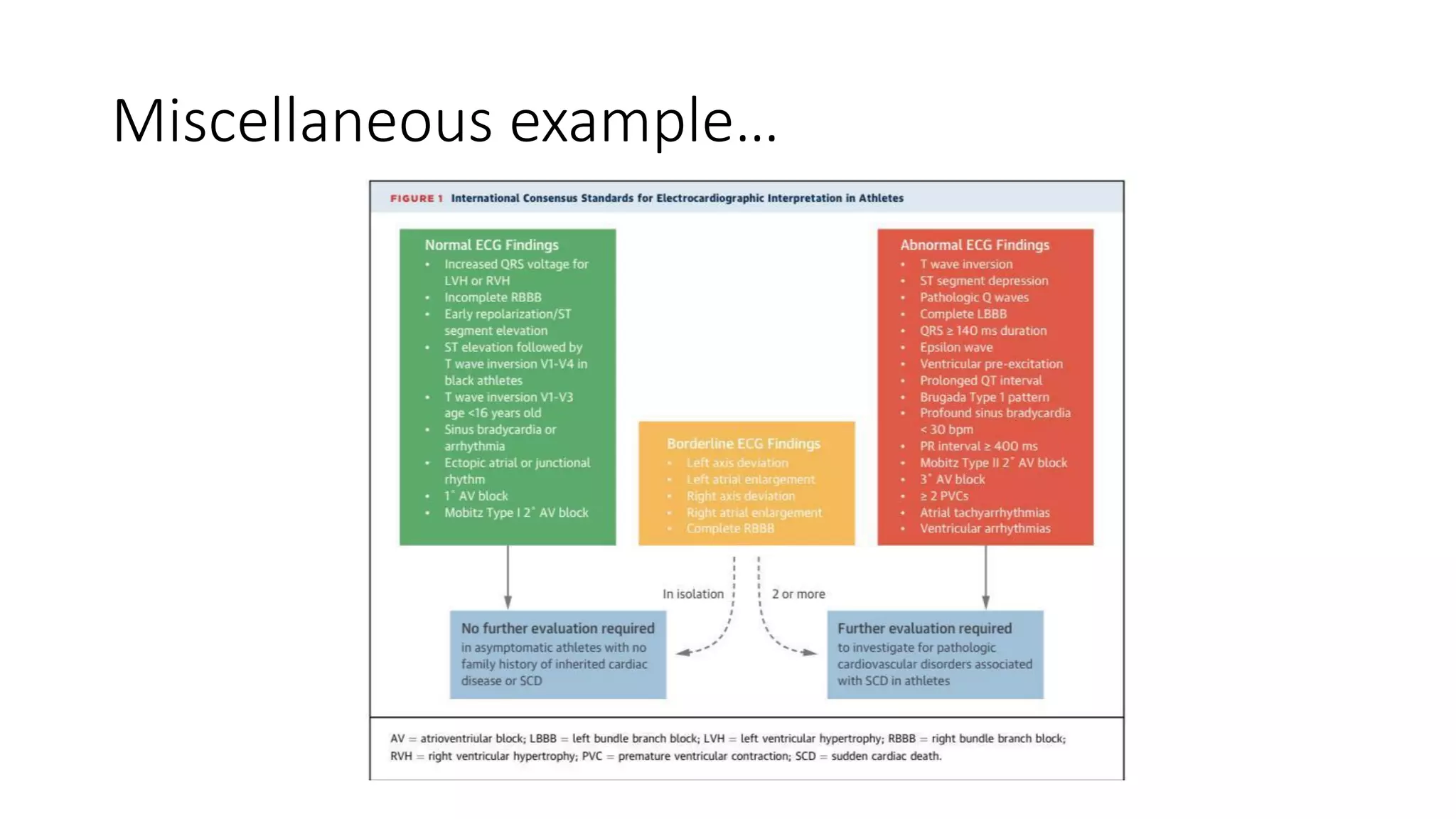
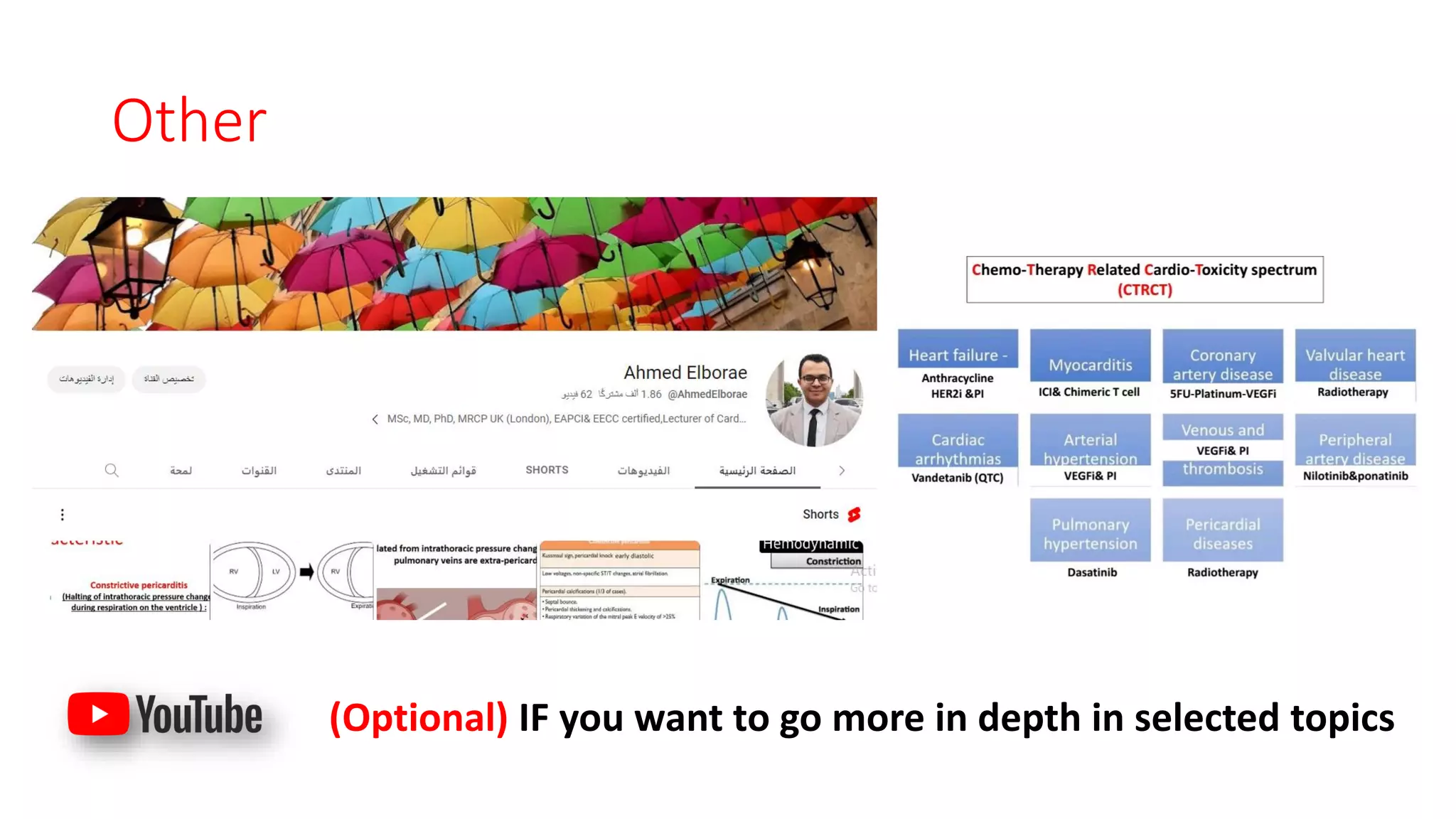
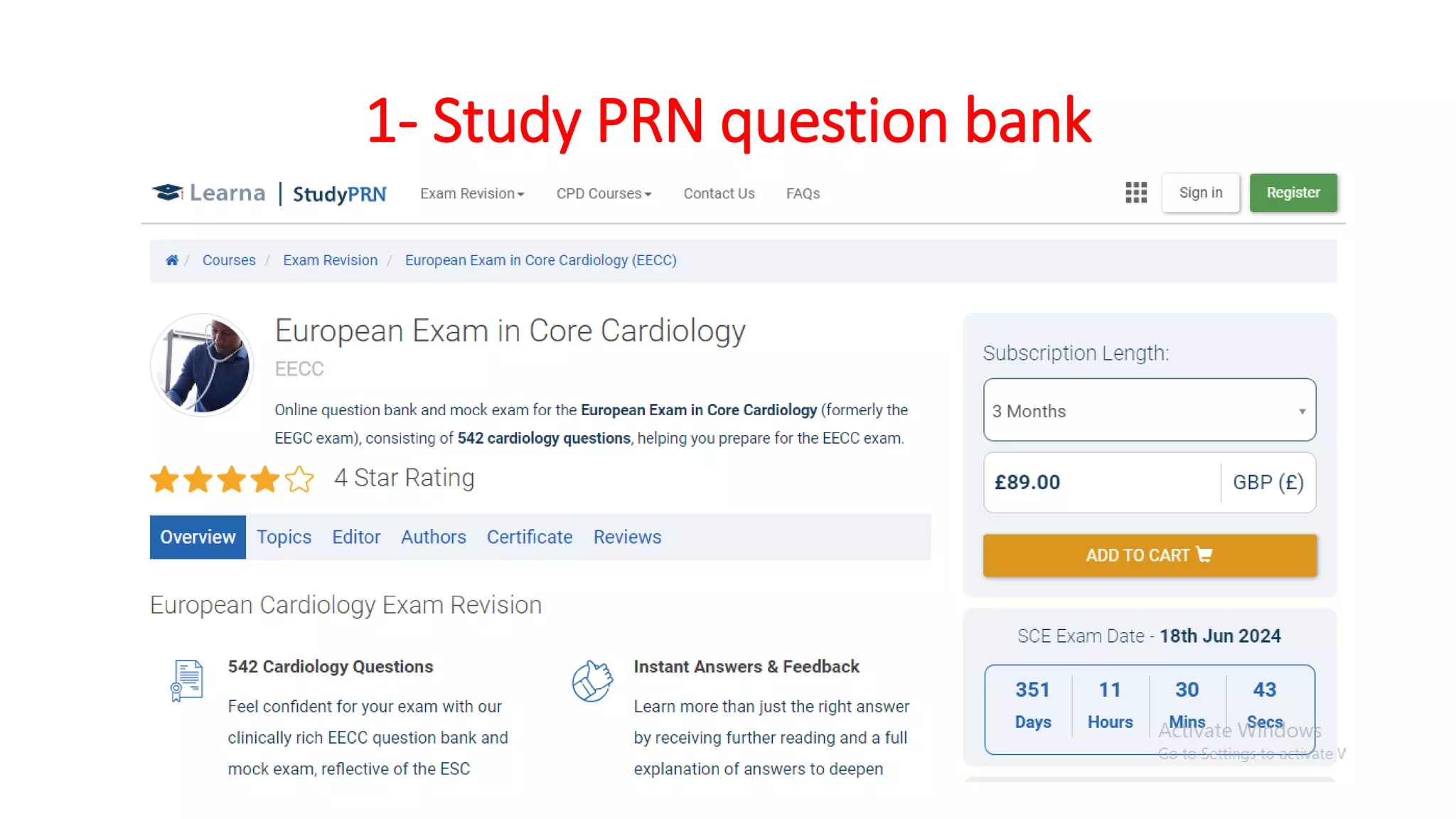
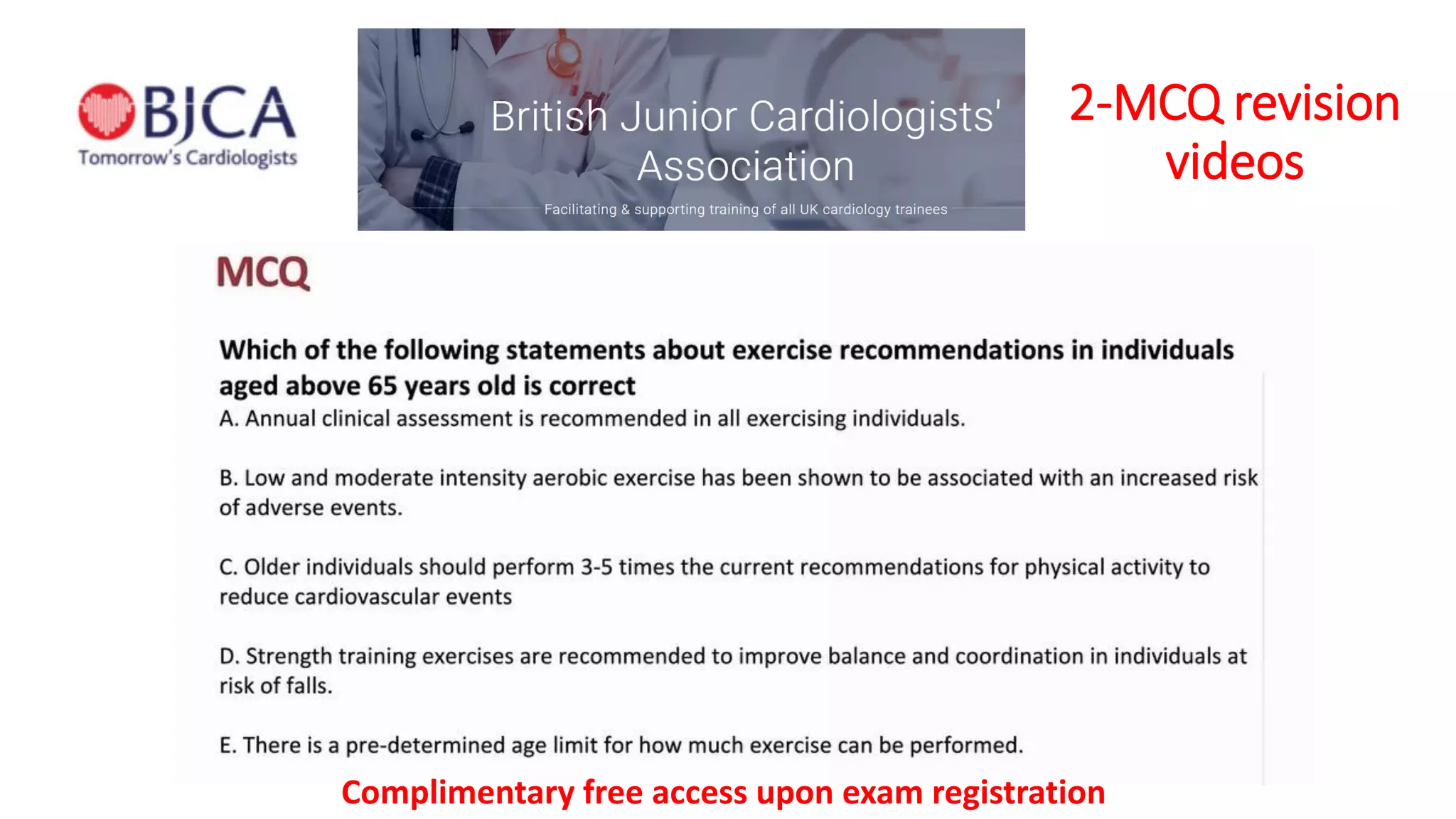
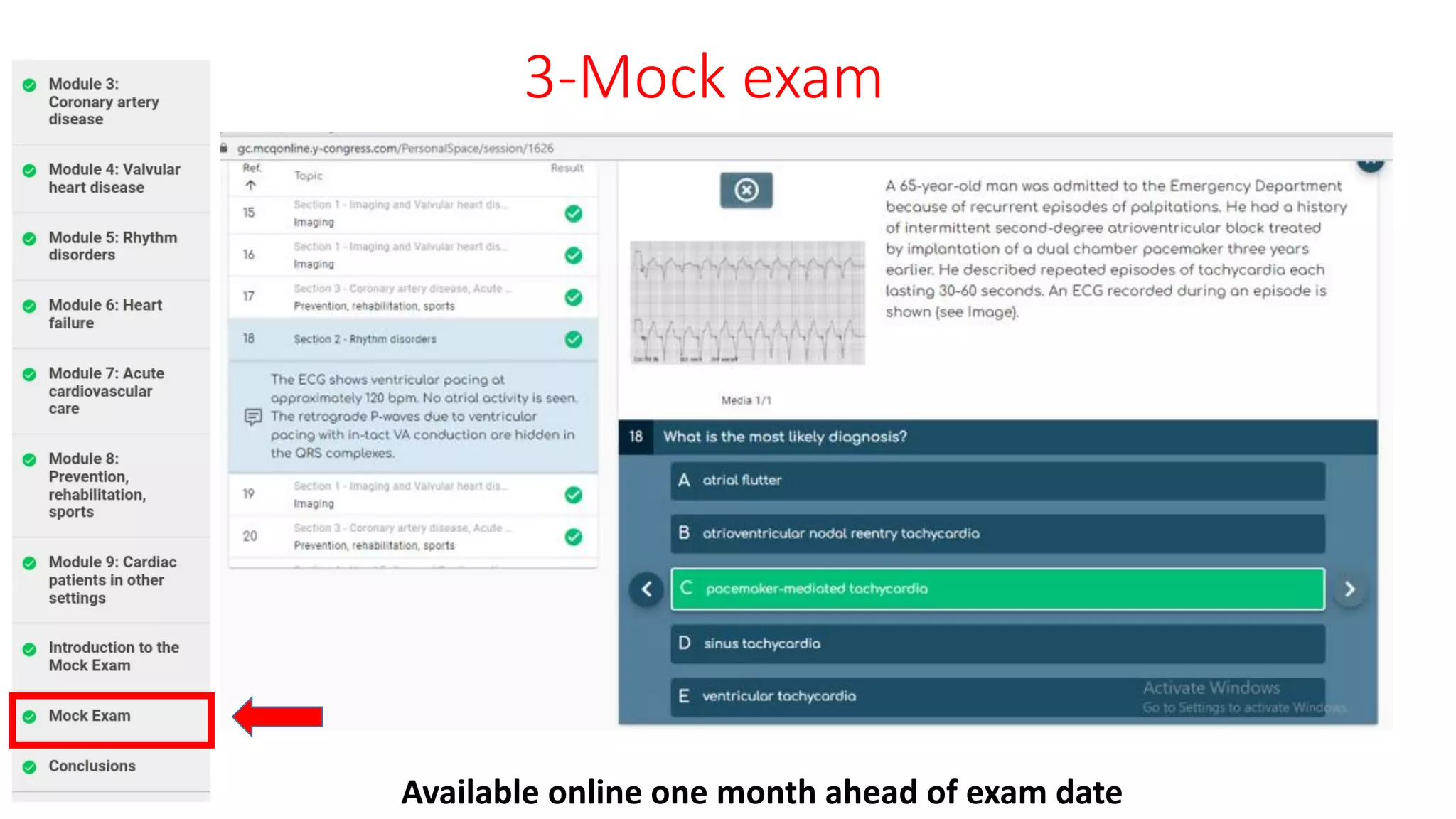
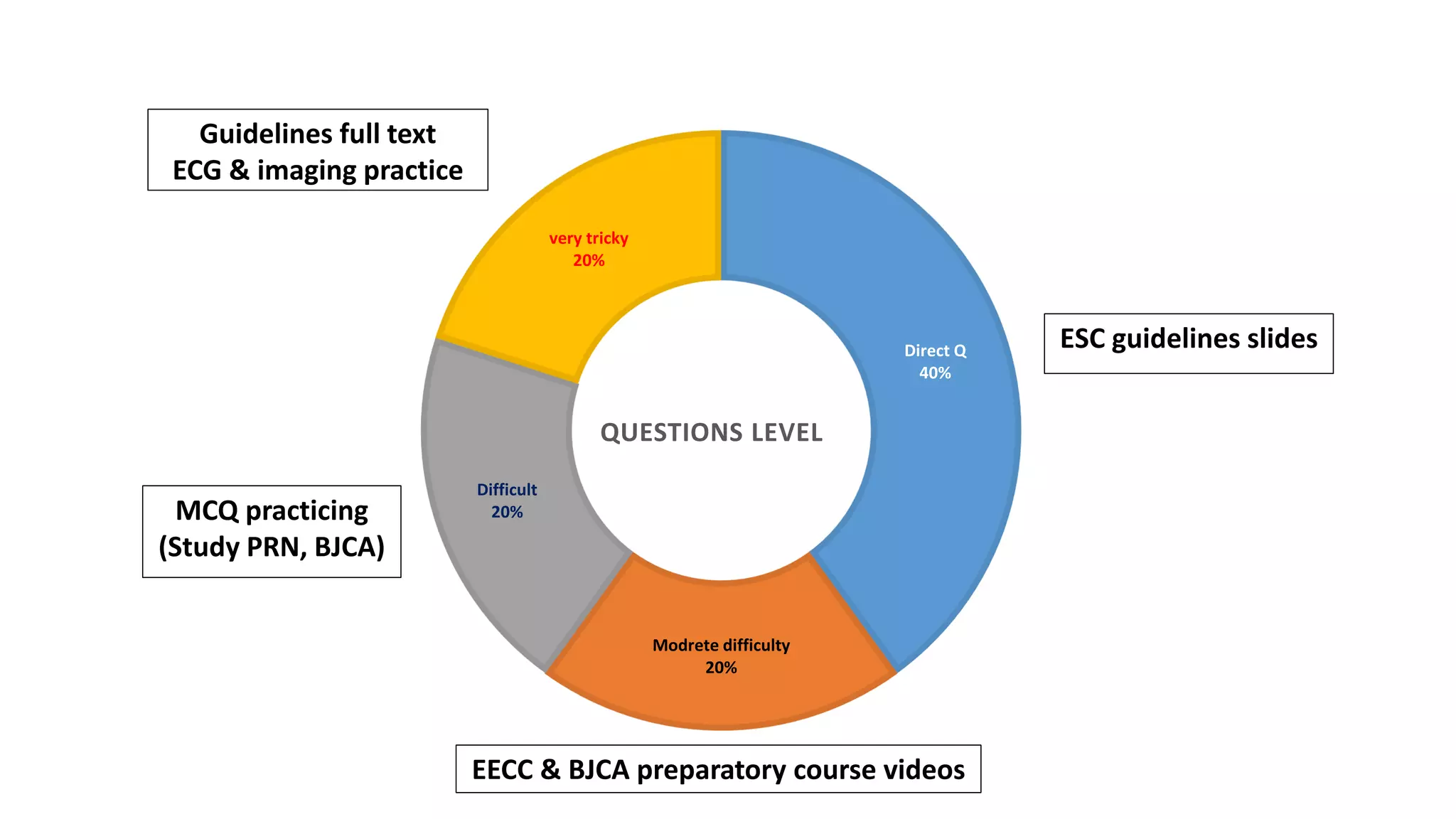
- Main resources for preparation include ESC Guidelines, the EECC free preparatory course, BJCA course, question banks, and mock exams. Guidelines and courses focus on algorithms, guidelines summaries, lectures, and imaging.
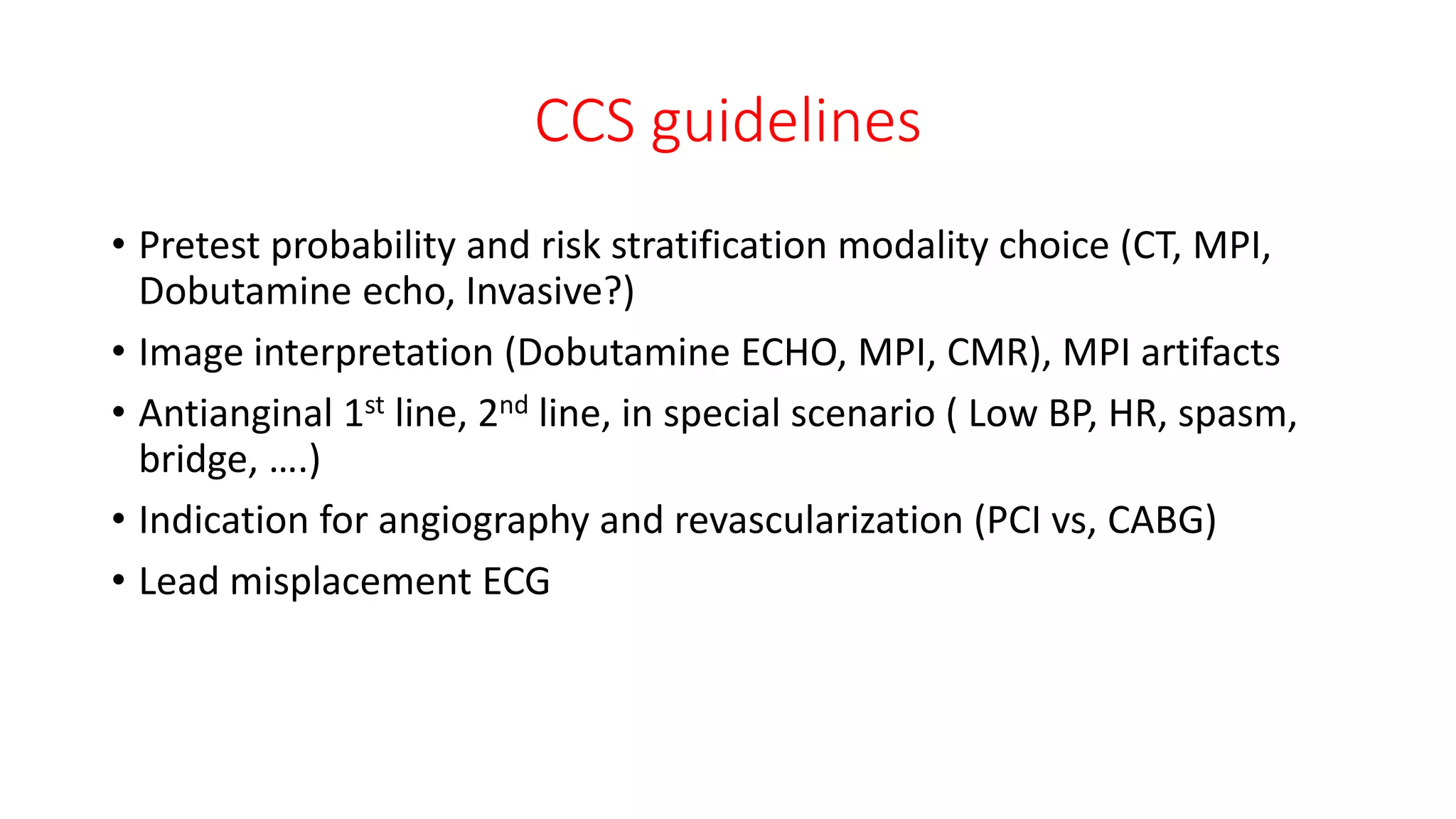
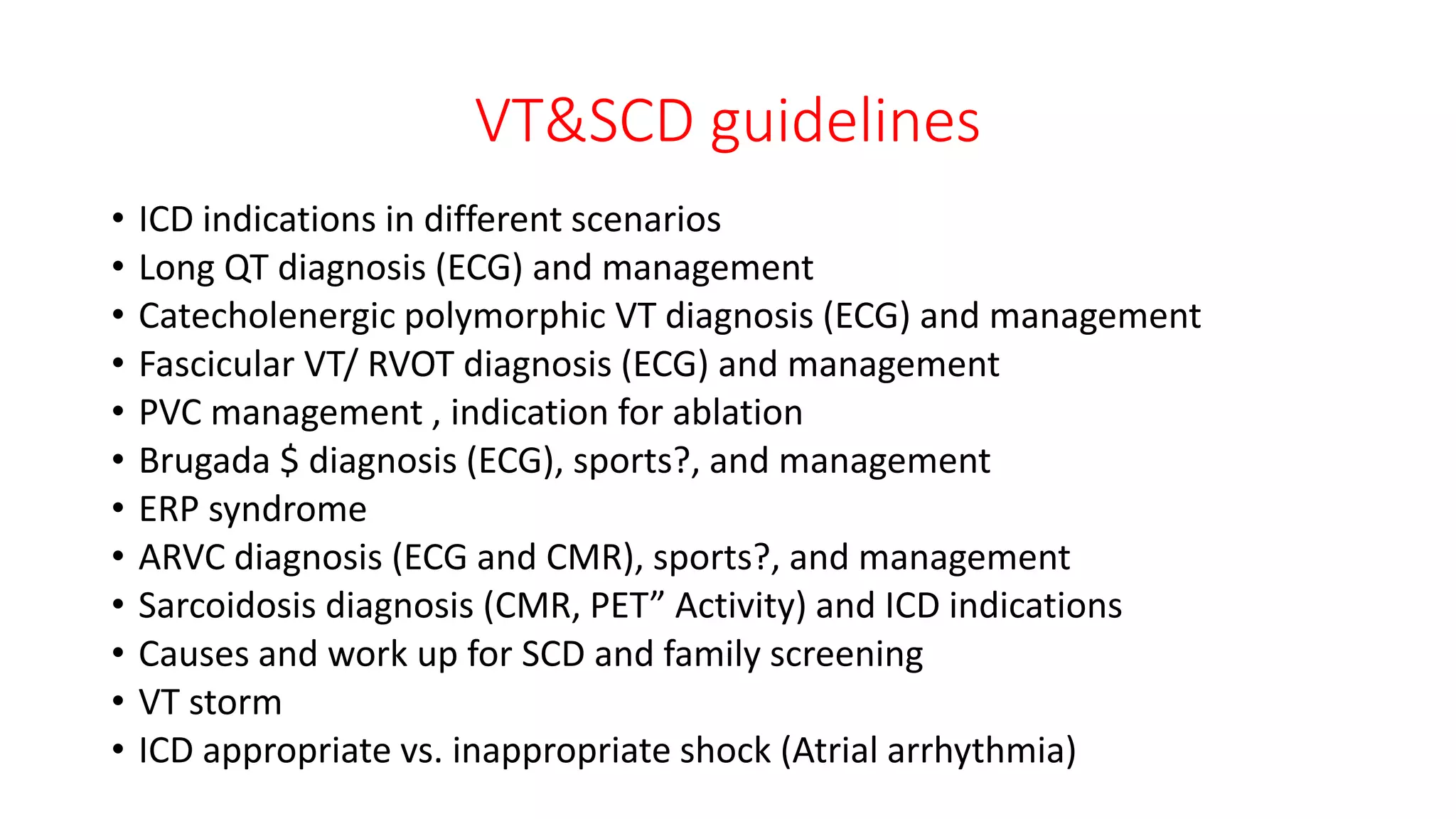
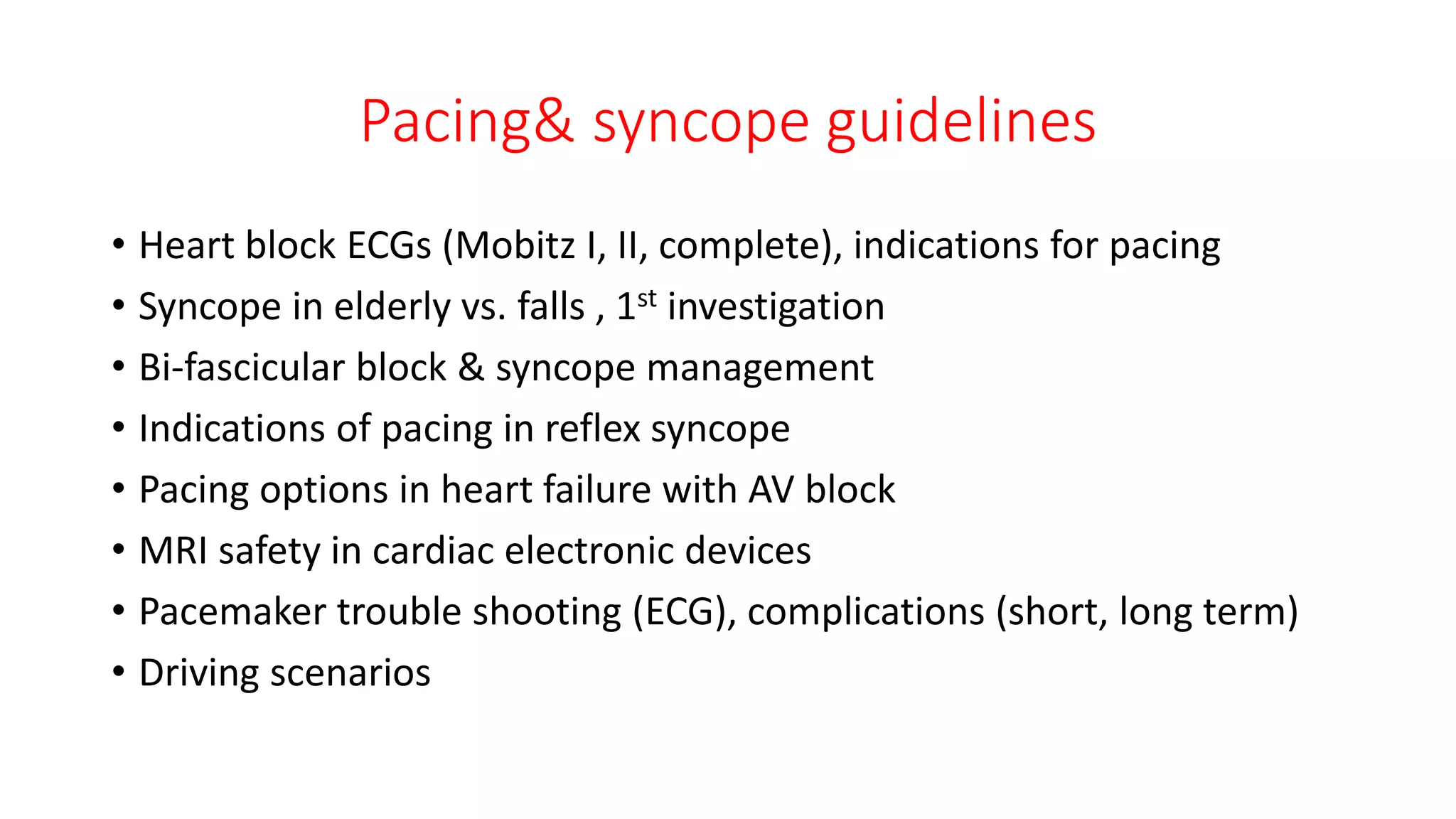
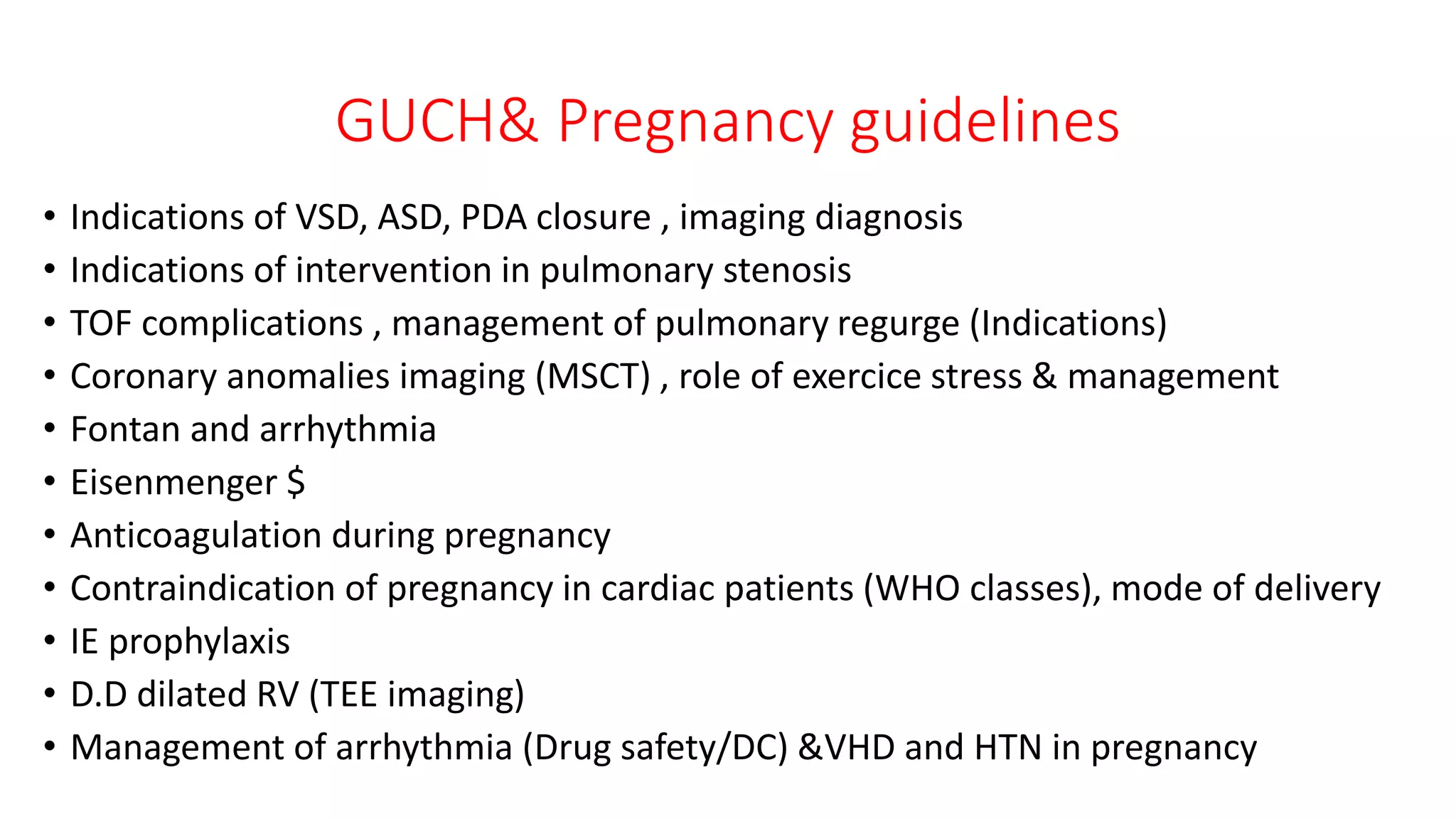
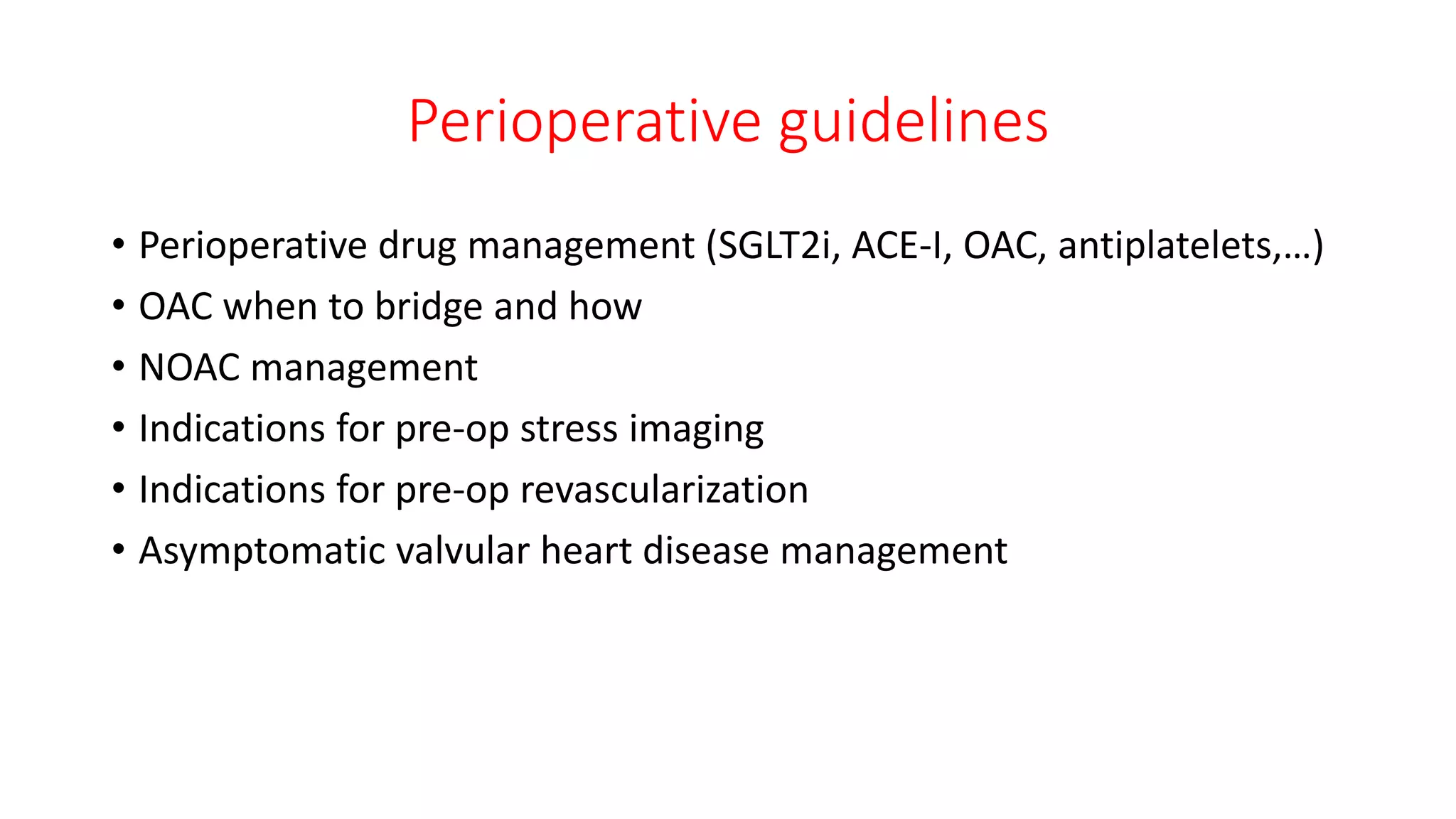
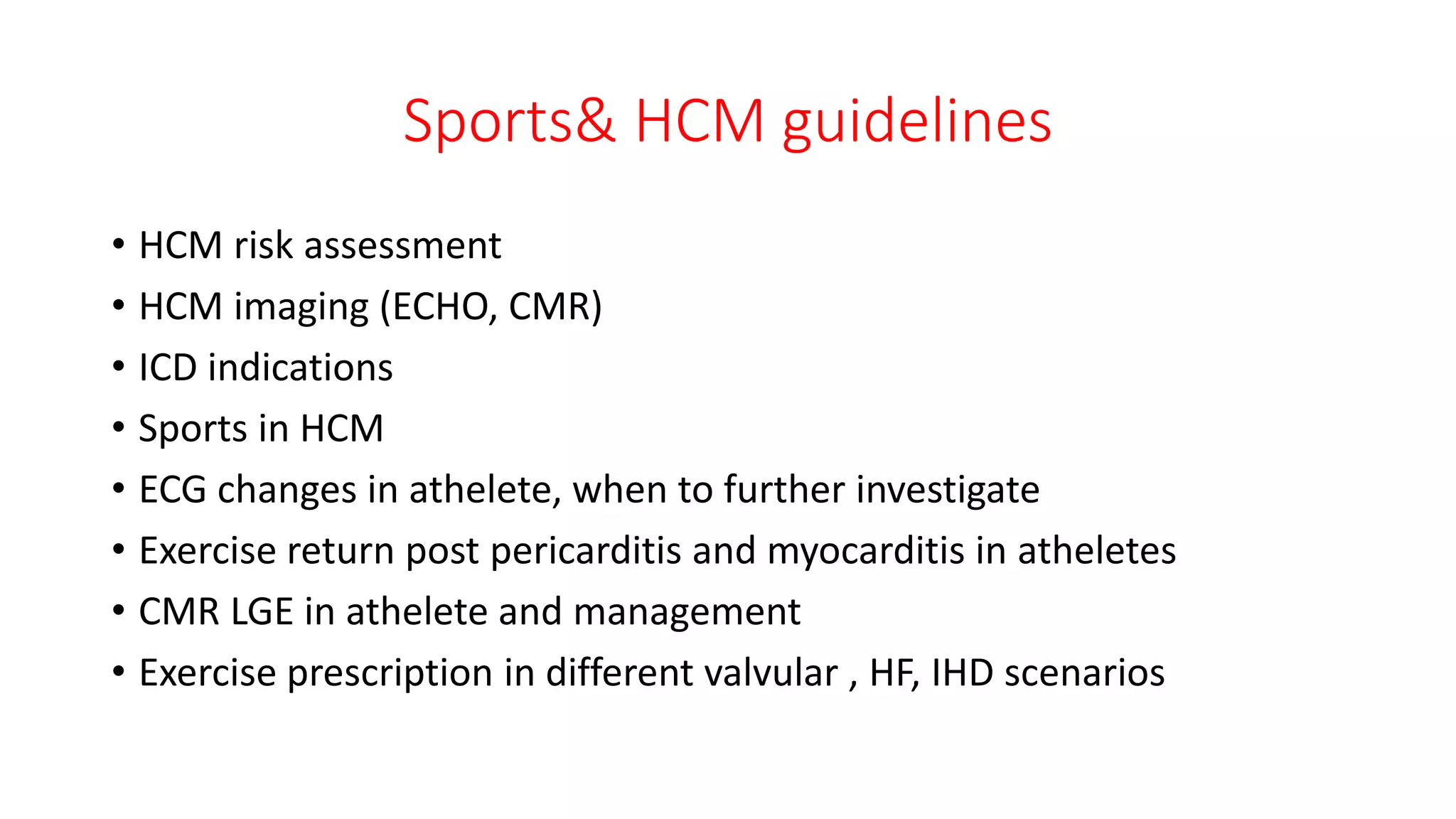
- Topics covered include heart failure, valvular disease, coronary artery disease, arrhythmias, and others. Guidelines should be reviewed