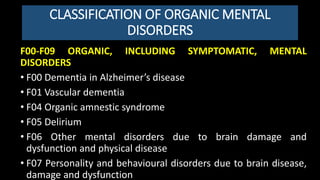
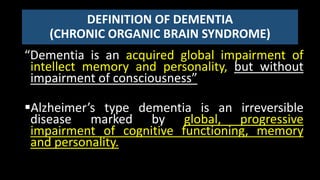
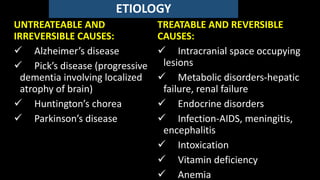
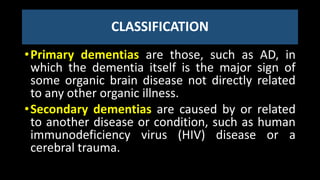
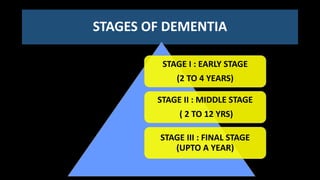
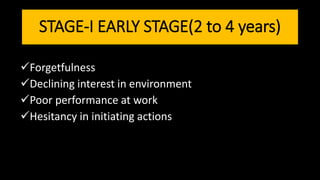
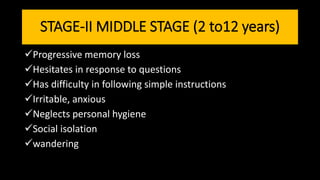
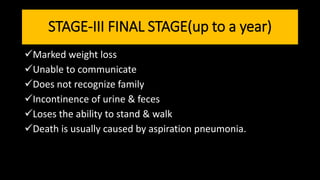
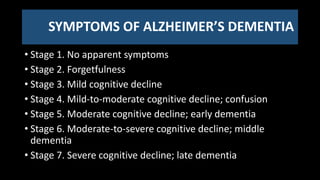
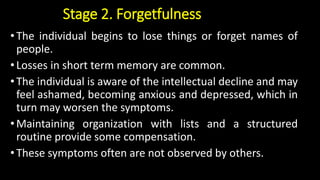
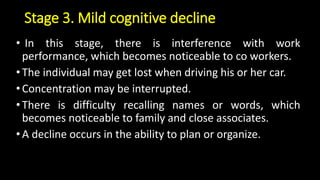
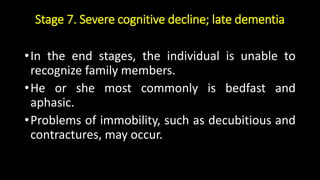
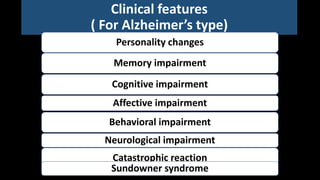
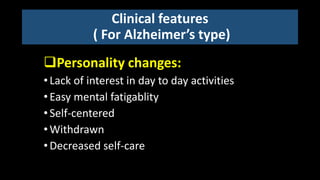
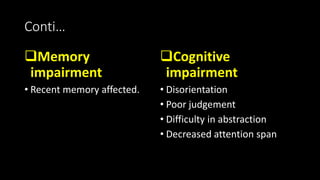
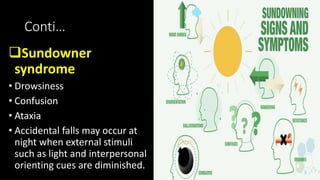
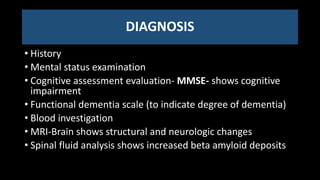
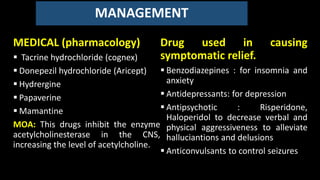
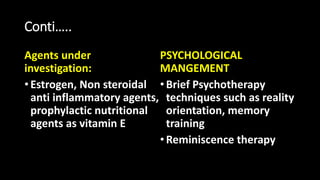
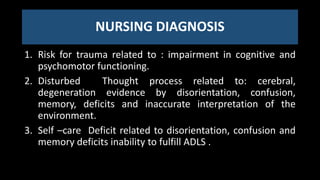
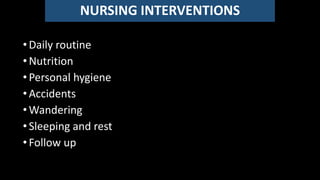
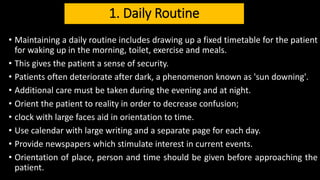
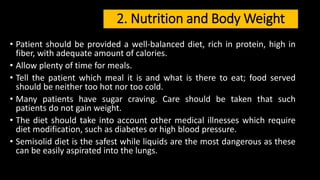
Organic brain disorders are behavioral or psychological disorders associated with transient or permanent brain dysfunction. This document discusses organic mental disorders including various types of dementia like Alzheimer's disease. It describes the classification, symptoms, stages, diagnosis and management of dementia. Dementia is characterized by global cognitive impairment without impaired consciousness. The incidence increases with age from 0.1% below 60 years to 15-20% for those over 80 years. Management involves both medical treatment to relieve symptoms as well as psychological and nursing care to support daily living.