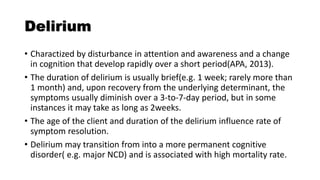
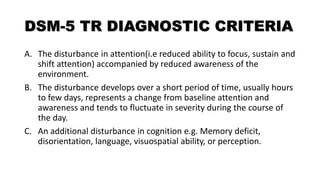
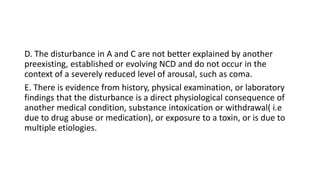
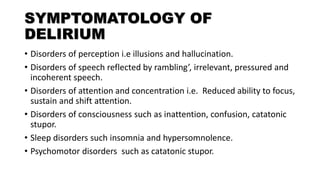
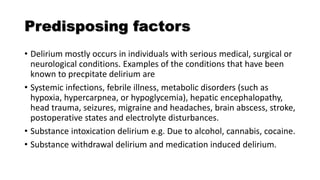
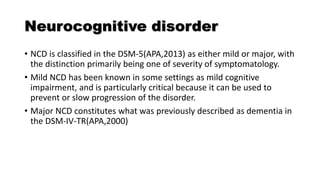
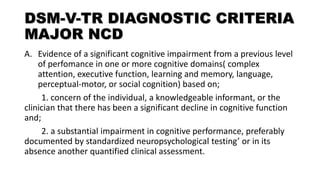
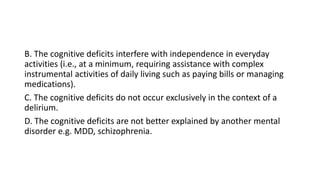
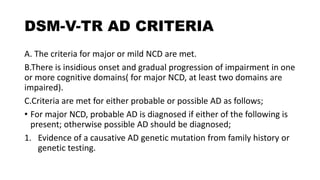
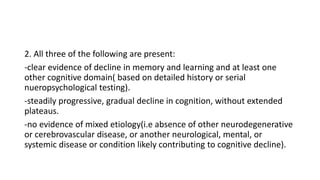
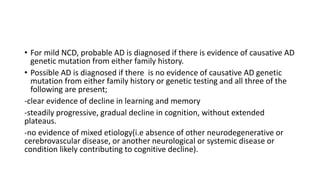
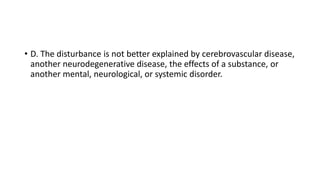
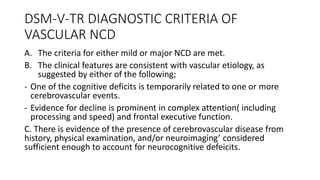
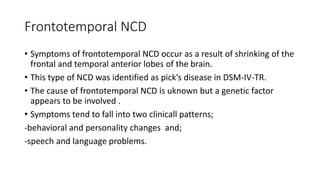
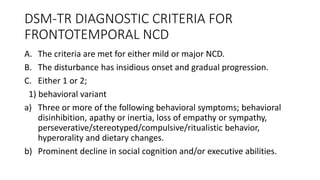
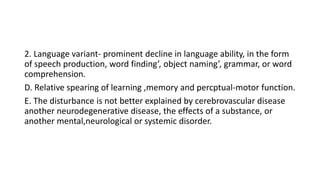
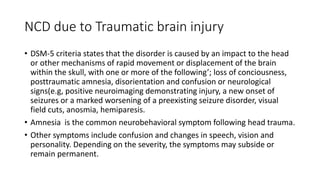
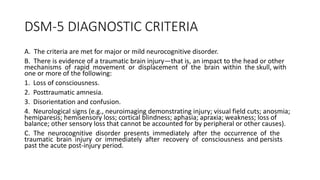
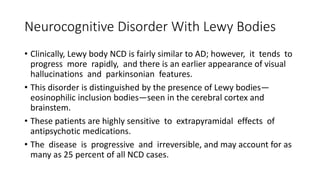
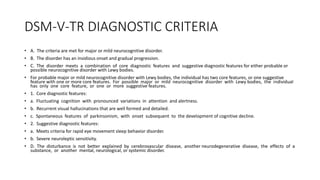
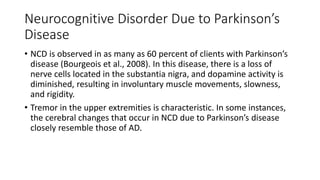
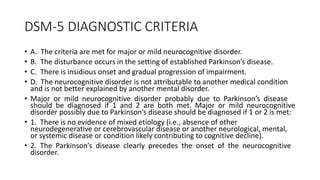
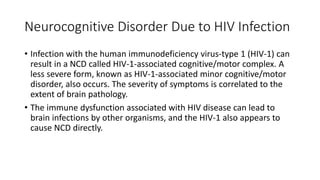
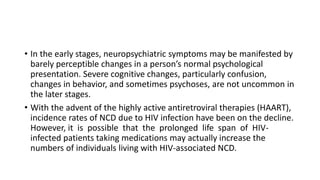
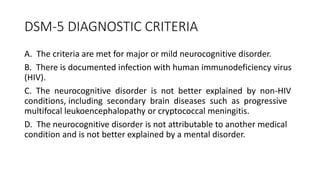
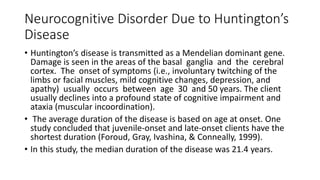
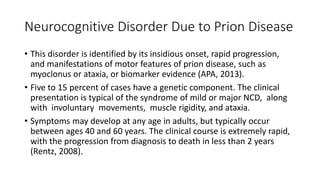
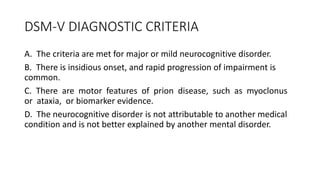
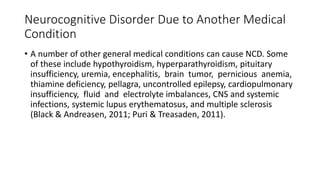
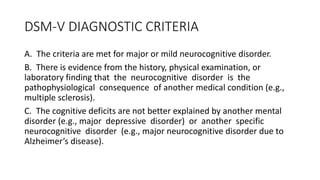
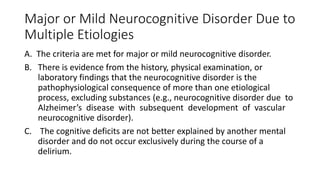
Neurocognitive disorders (NCDs) include conditions involving significant cognitive decline from previous levels of functioning. Major subtypes include those due to Alzheimer's disease, vascular factors, Lewy bodies, Parkinson's disease, frontotemporal deficits, traumatic brain injury, HIV, Huntington's disease, prion disease, or multiple etiologies. Delirium is characterized by acute changes in attention and cognition. Diagnosis of major or mild NCD due to conditions like Alzheimer's disease requires evidence of cognitive impairment in multiple domains interfering with daily life. Vascular NCD results from cerebrovascular disease and impairment occurs in step-like progression following small strokes in the brain.