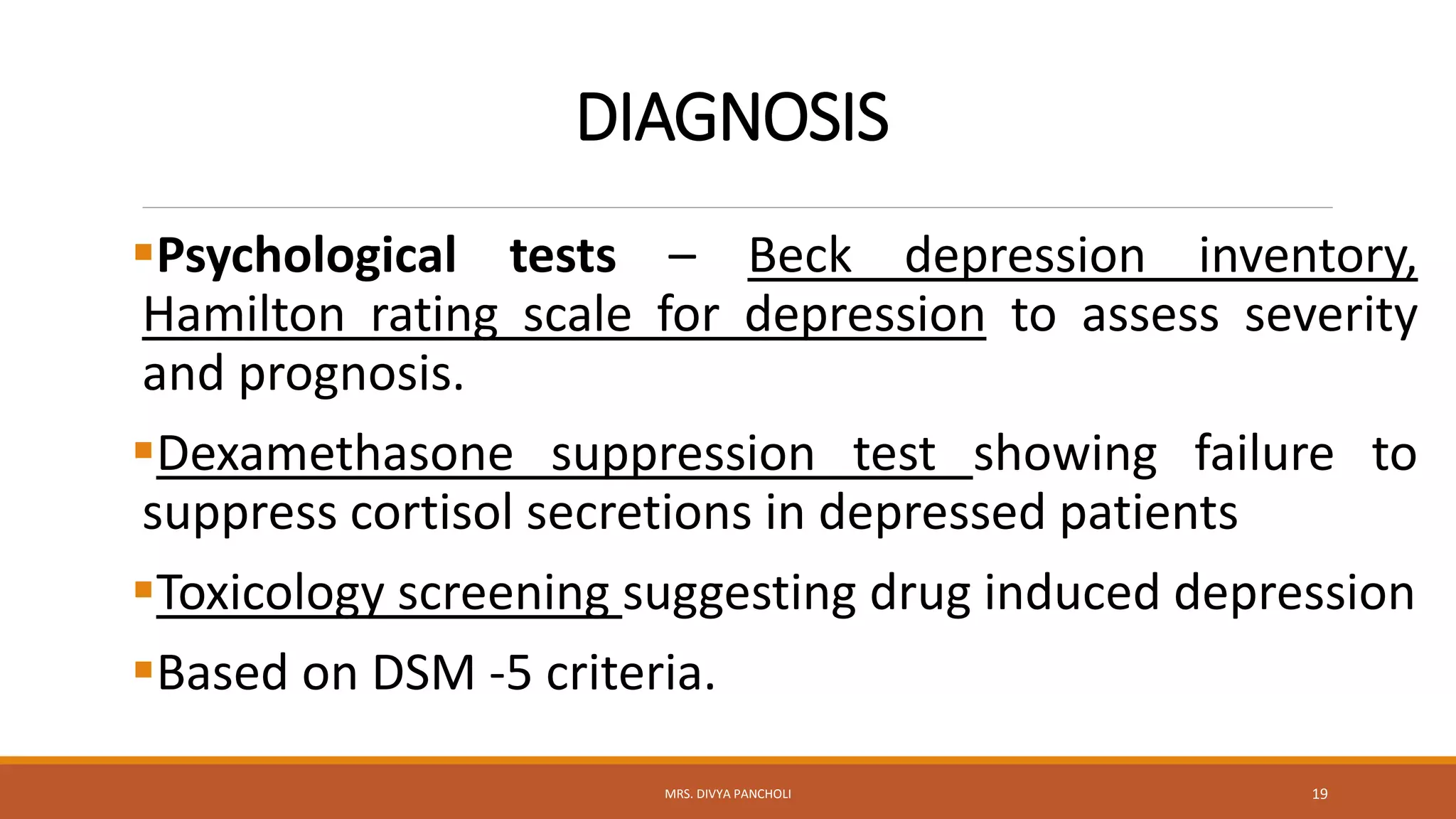
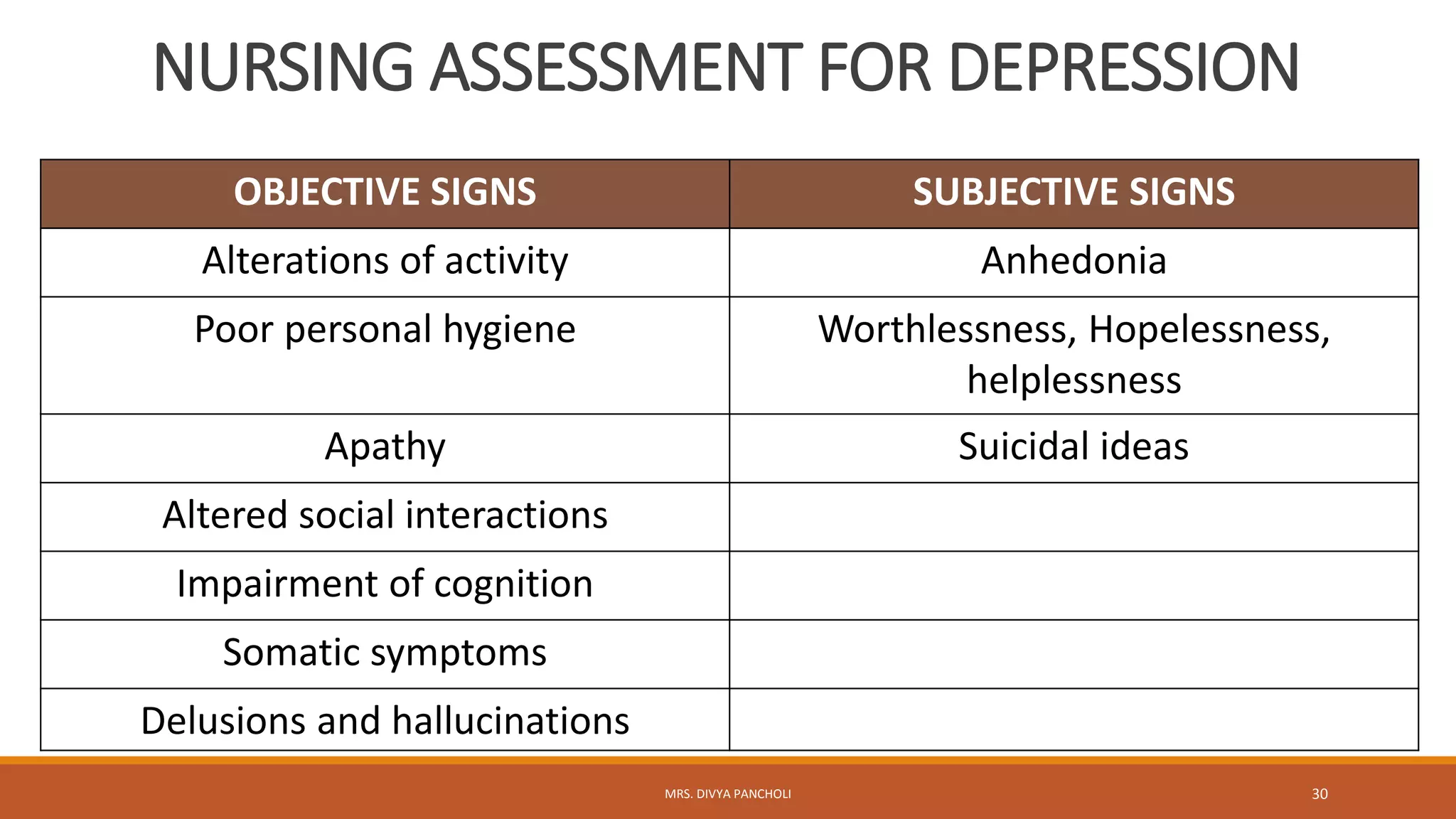
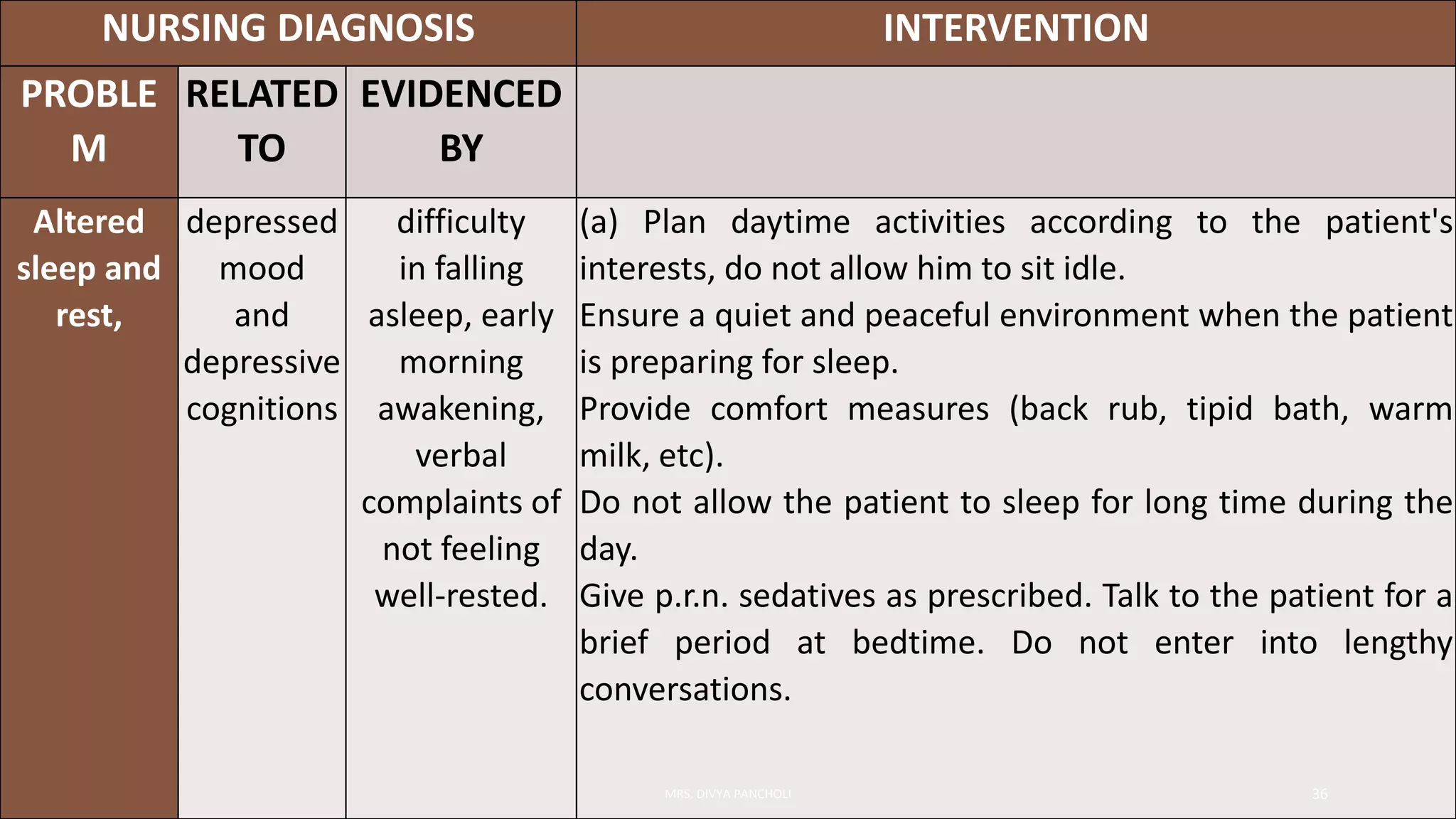
Depression is an alteration in mood characterized by sadness, despair, and loss of interest in usual activities. It commonly affects sleep and appetite. The incidence is higher in women and those who are divorced or separated. It can be mild, moderate, severe, or with psychotic features. Potential causes include biological factors like neurotransmitter levels, genetics, hormones, and brain changes as well as psychological and social stressors. Symptoms include depressed mood, low self-esteem, guilt, impaired thinking, and suicidal thoughts. Treatment involves antidepressant medication, psychotherapy, electroconvulsive therapy, and addressing needs like nutrition, sleep, and social support. Nurses monitor for safety and suicide risk, help patients meet basic needs, and provide