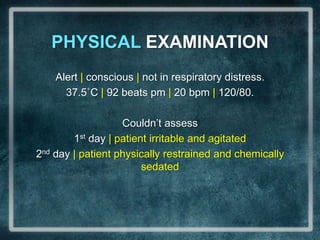
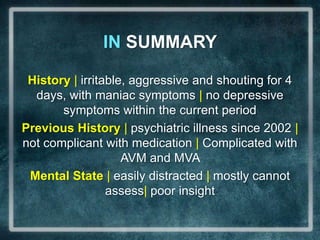
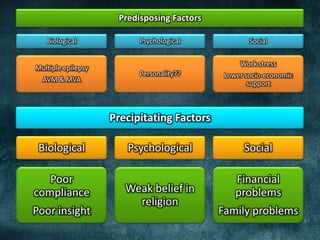
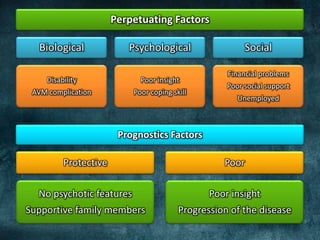
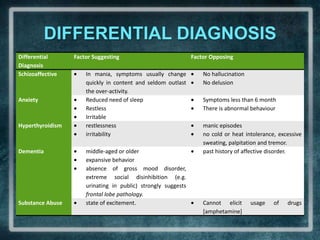
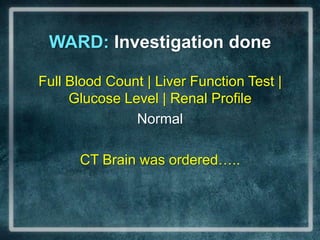
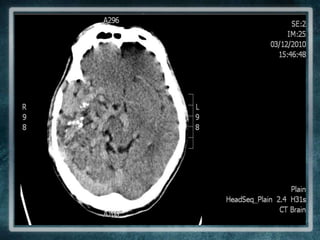
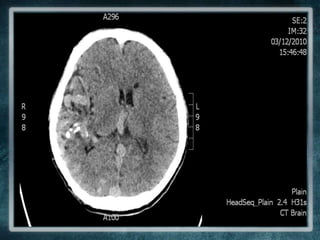
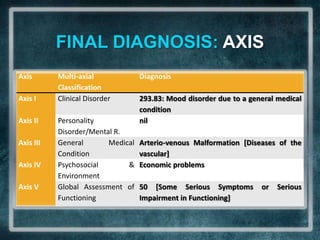
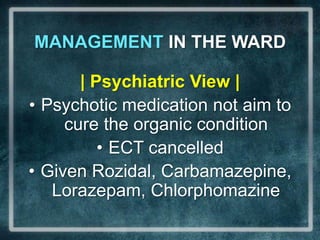
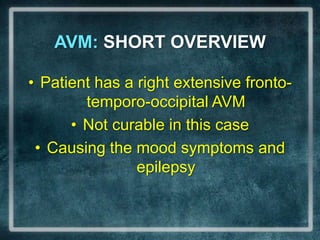
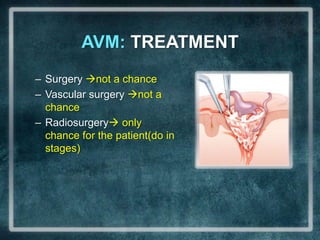
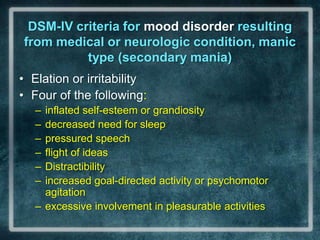
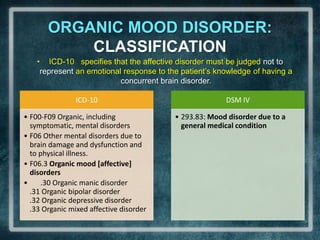
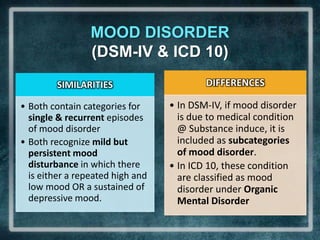
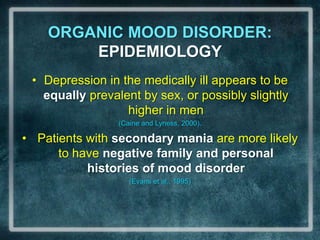
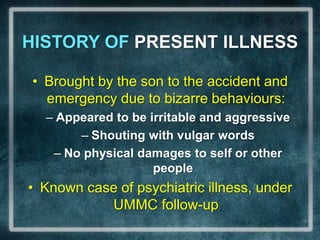
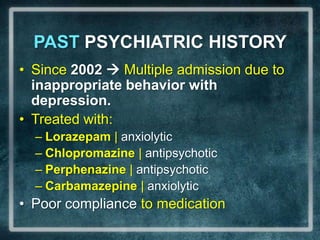
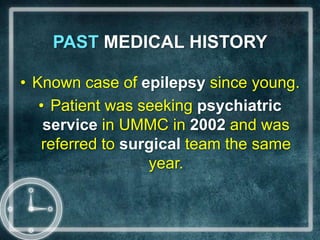
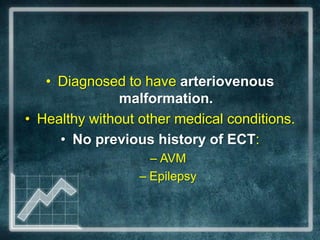
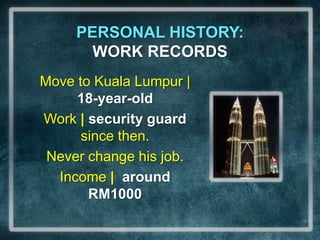
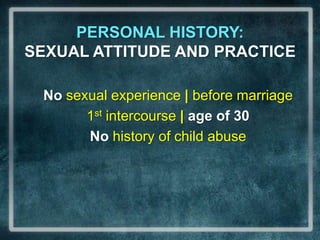
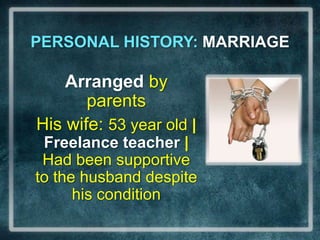
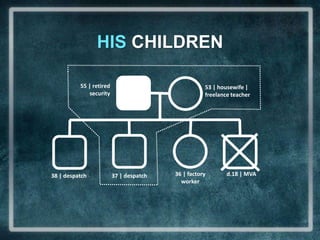
The document discusses the case of a 55-year-old male security guard with a history of psychiatric illness and recent manic symptoms. He exhibited aggressive and bizarre behavior over four days, with a past medical history including arteriovenous malformation and epilepsy. Provisional diagnosis suggests bipolar I disorder with a manic episode, linked to organic mood disorder due to his complex neurological condition.
![PAST PSYCHIATRIC HISTORY8/02Sm: Abnormal behaviour & EpilepsySurgDx: AVM1/06, 7/06, 12/06Multiple admission on Epilepsy10/09Motor Vehicle accident: cross the highway |polytrauma[contusion, haemothorax, SDH, AVM Current Admission 2005 2006 2007 2008 2009 201012/05Sm: ↓ need of sleep, aggressive [shouting]19/8 – 21/9Stressor: stolen motor,Fired from jobSm: shouting to family, aggitated10/09After operation: ruptured diagphragm with right upper limb fracture](https://image.slidesharecdn.com/caseconferencefinal-101212223422-phpapp02/85/Organic-Mood-Disorder-and-AVM-8-320.jpg)
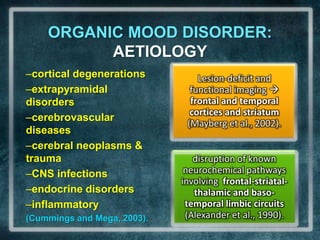
![MENTAL STATE: COGNITIVE FUNCTIONTime, Place, Person | OrientatedRemote, Recent Memory | Good[date of birth & breakfast]5mins memory test | Remember only 1Information/knowledge | AppropriateProverbs | Can answer [Udang di sebalikbatu & sikit-sikit lama-lama jadibukit]Similarities | Give 2[apple & orange: tastes, eaten]](https://image.slidesharecdn.com/caseconferencefinal-101212223422-phpapp02/85/Organic-Mood-Disorder-and-AVM-25-320.jpg)
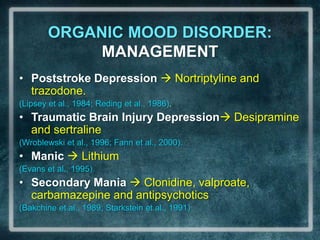
![MENTAL STATE: COGNITIVE FUNCTION 2Attention | Easily distractedConcentration | Cant do it[serial 7 test, digit span, world backward]Judgement | Cant assess[patient started irritable and agitated]Insight | Poor [he and others do not realised his abnormality | not accept and do not need treatment]](https://image.slidesharecdn.com/caseconferencefinal-101212223422-phpapp02/85/Organic-Mood-Disorder-and-AVM-26-320.jpg)