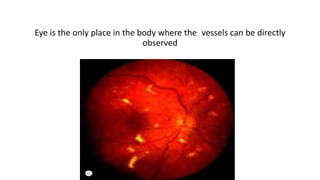
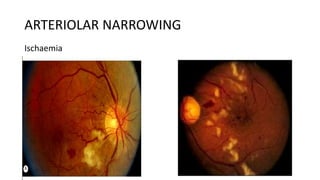
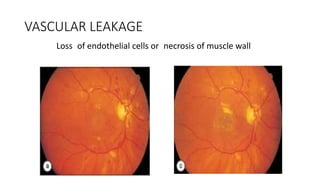
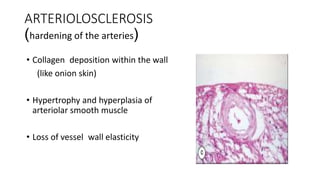
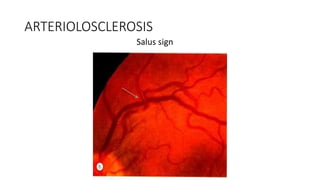
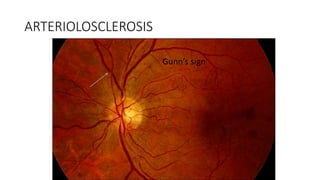
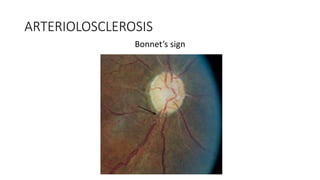
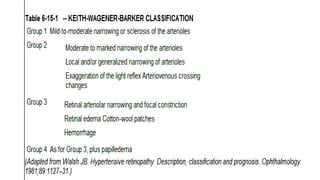
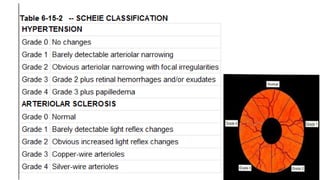
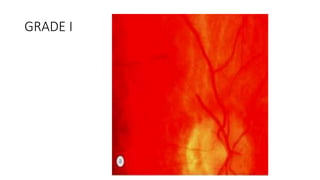
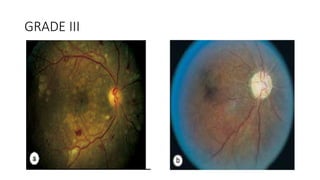
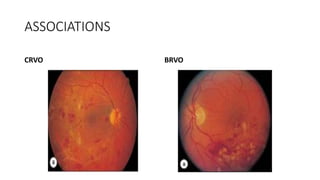
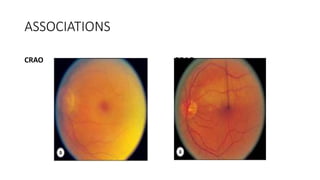
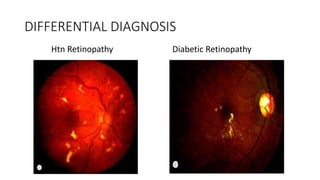
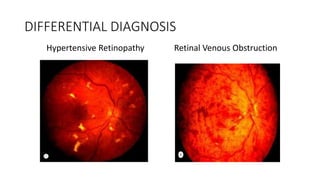
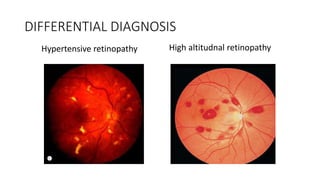
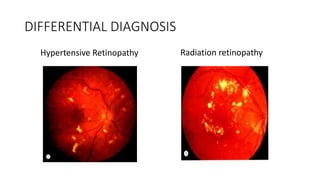
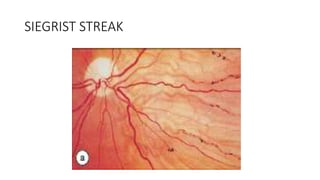
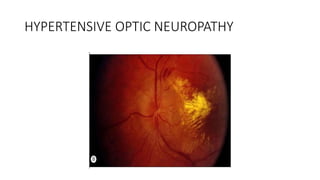
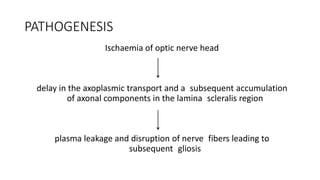
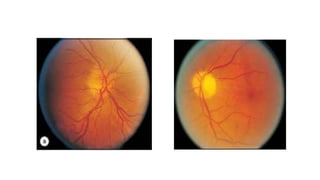
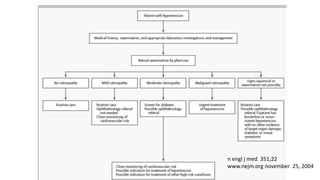
This document discusses hypertensive retinopathy, which refers to retinal vascular changes caused by high blood pressure. It notes that the prevalence of hypertensive retinopathy is approximately 15% among hypertensive patients without other vascular diseases. The key signs include arteriolar narrowing, arteriovenous nicking, and cotton wool spots. The pathogenesis involves initial vasoconstriction, then exudation and fluid leakage due to damaged blood vessels, and finally arteriolar sclerosis. Hypertensive choroidopathy and optic neuropathy can also occur in severe untreated cases and are characterized by lesions such as Elsching spots. Strict blood pressure control and regular eye screening are important for treatment and prevention of further vision loss