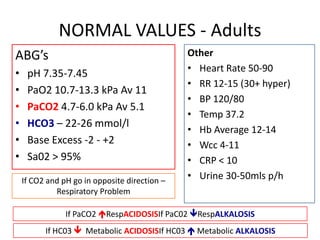
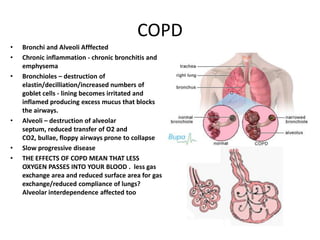
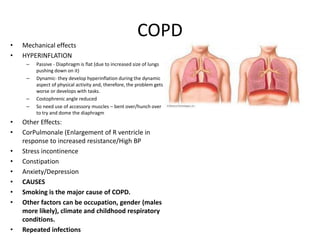
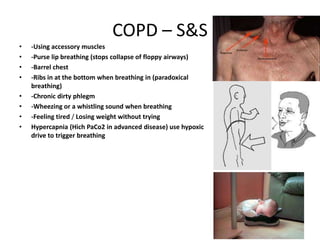
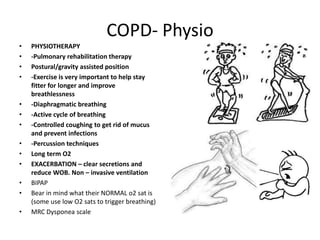
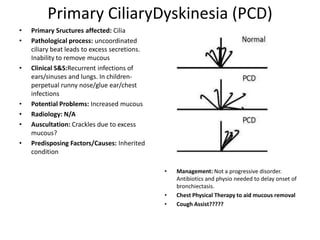
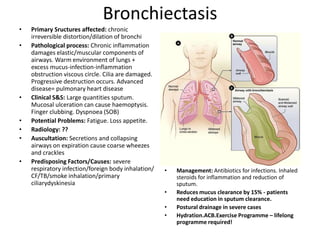
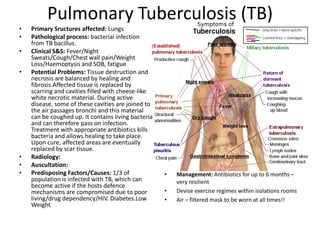
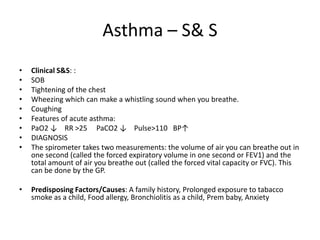
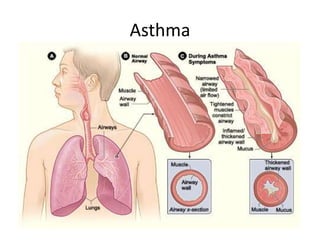
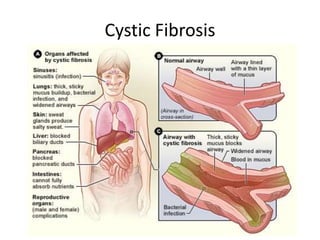
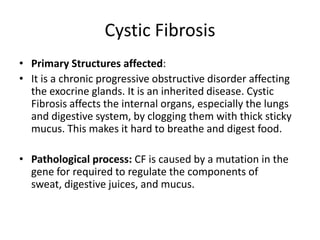
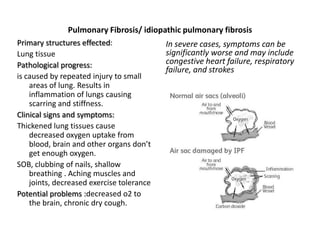
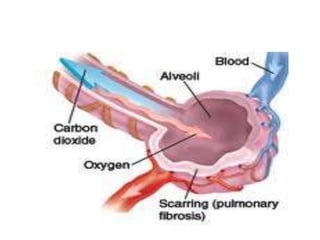
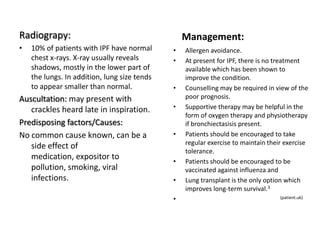
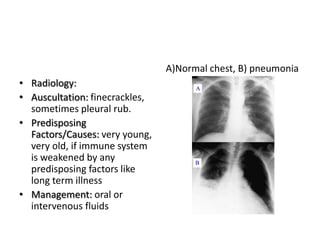
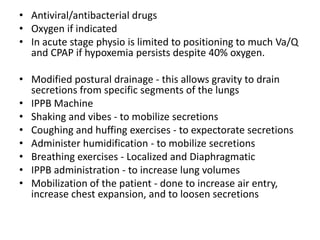
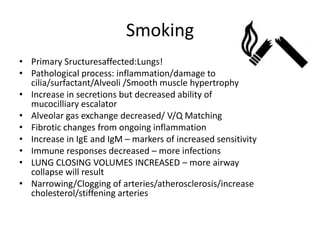
The document provides information on various pulmonary conditions including normal adult ABG values, COPD, asthma, bronchiectasis, primary ciliary dyskinesia, pulmonary tuberculosis, and their signs and symptoms, pathophysiology, predisposing factors, radiology findings, auscultation findings, potential complications, and management including medications, physiotherapy, exercise programs, and lifestyle changes. Conditions discussed include the structures affected, causes of inflammation and airway obstruction, and methods to reduce symptoms and exacerbations through airway clearance techniques and antibiotic treatment of infections.