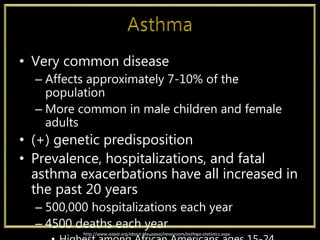
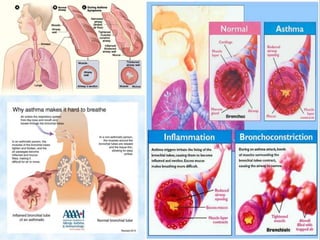
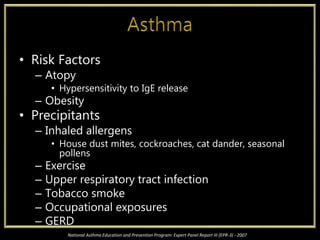
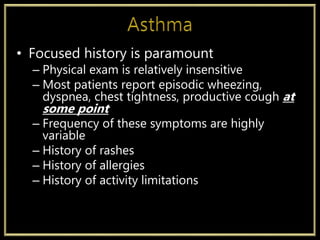
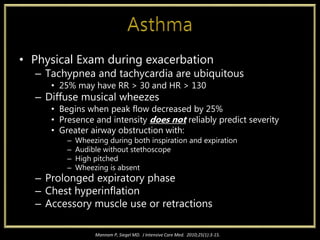
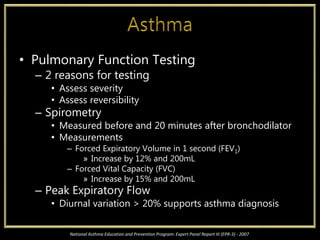
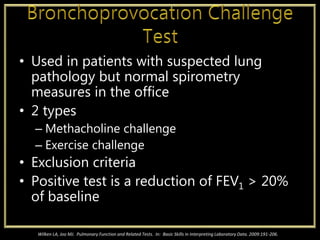
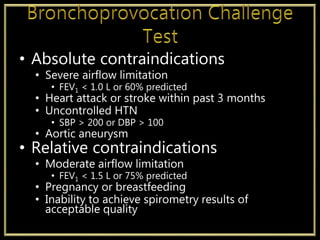
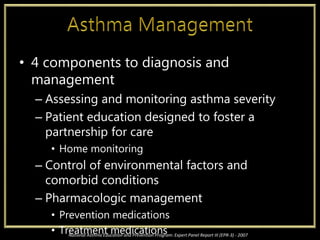
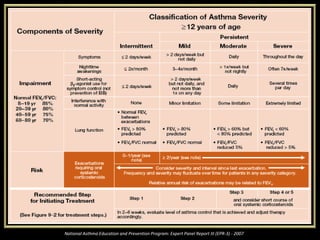
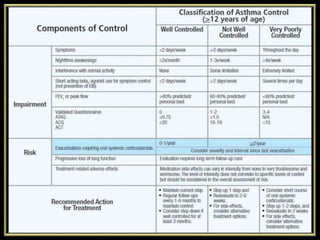
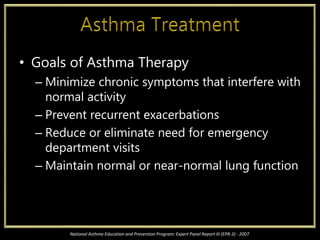
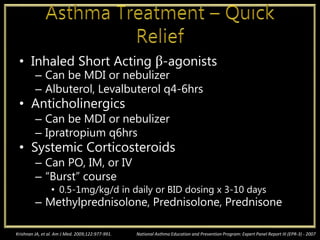
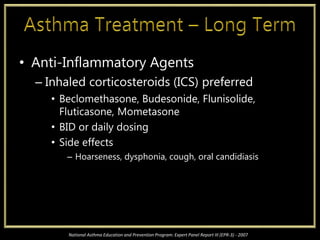
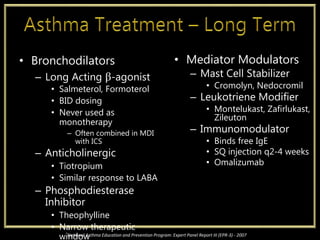
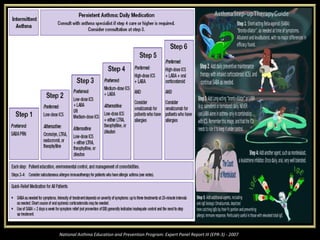
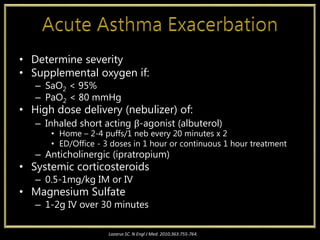
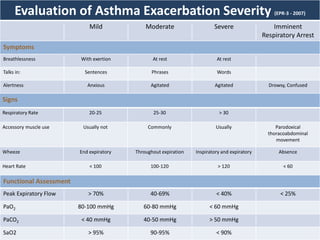
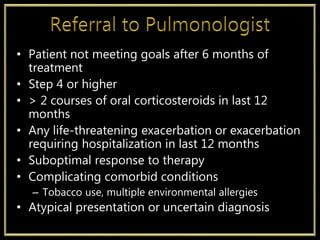
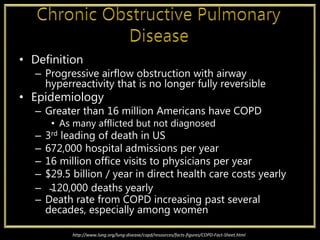
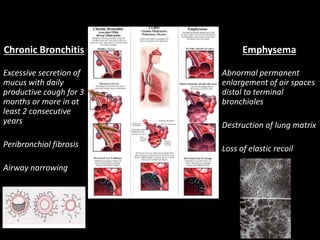
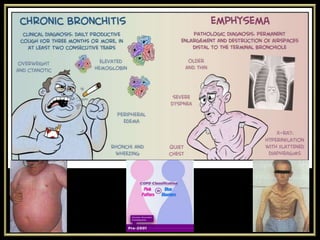
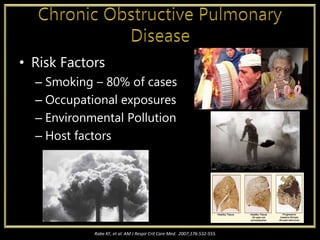
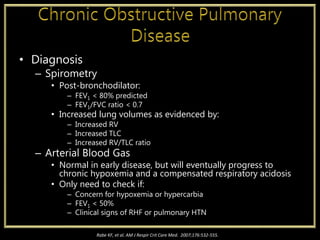
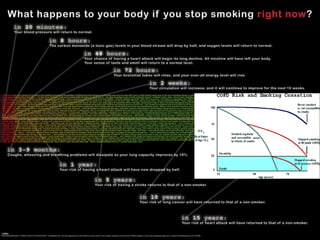
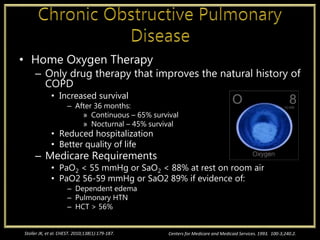
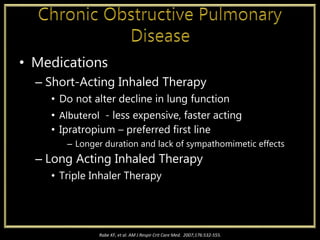
This document discusses chronic bronchitis and asthma. It provides information on the definition, epidemiology, risk factors, signs and symptoms, diagnosis, and treatment of each condition. For chronic bronchitis, key points include that it is progressive airflow obstruction, affects over 16 million Americans, and smoking is the primary risk factor. Asthma affects 7-10% of the population and prevalence has increased in recent decades. Diagnosis involves assessing severity, controlling triggers, and pharmacological management. Treatment focuses on minimizing symptoms and exacerbations through the use of bronchodilators and anti-inflammatory medications.