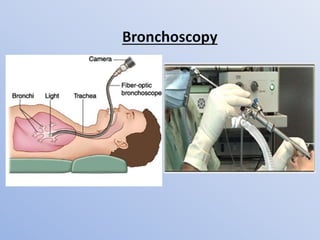
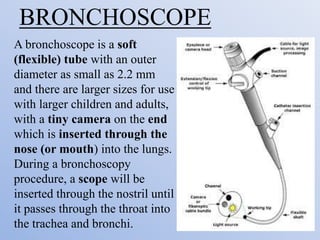
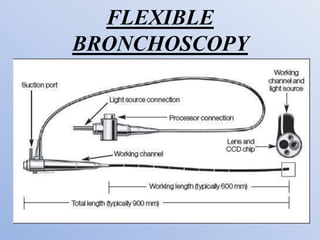
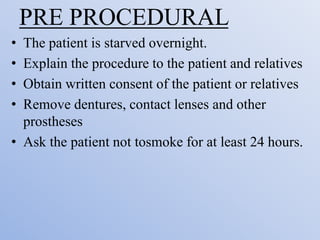
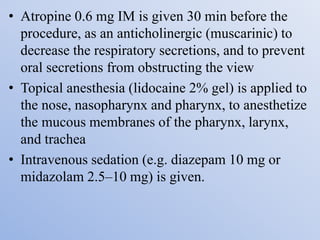
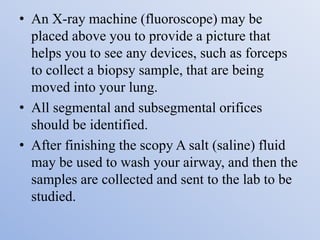
Bronchoscopy is a procedure that uses a thin, flexible tube called a bronchoscope to examine the airways. The bronchoscope is inserted through the nose or mouth and into the lungs. This allows doctors to visually examine the lungs for abnormalities and take samples. Bronchoscopy can be used for both diagnostic purposes to examine the lungs as well as therapeutic purposes, such as removing tumors or foreign objects from the airways. The procedure involves sedation of the patient and monitoring during insertion and examination of the lungs.