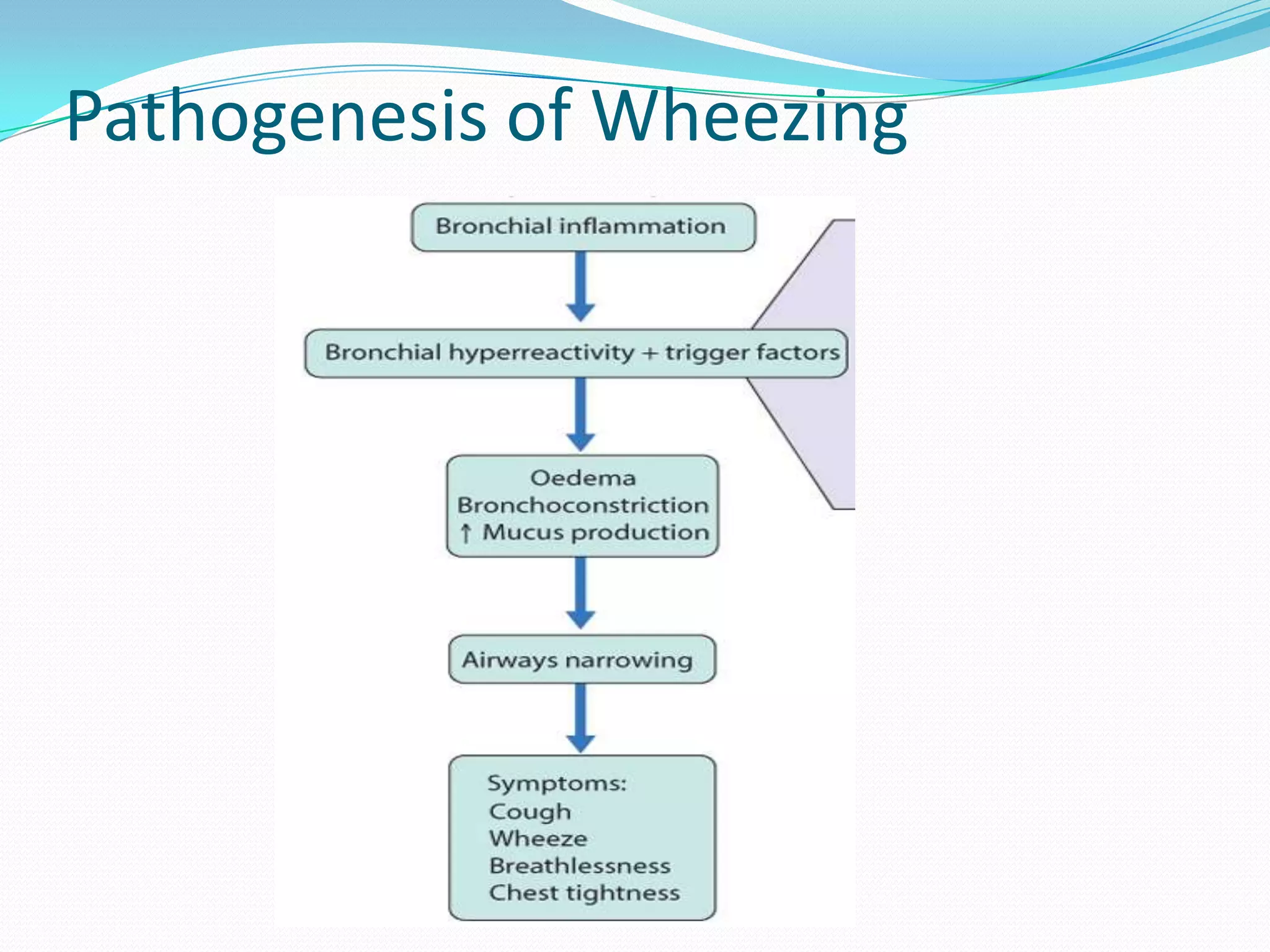
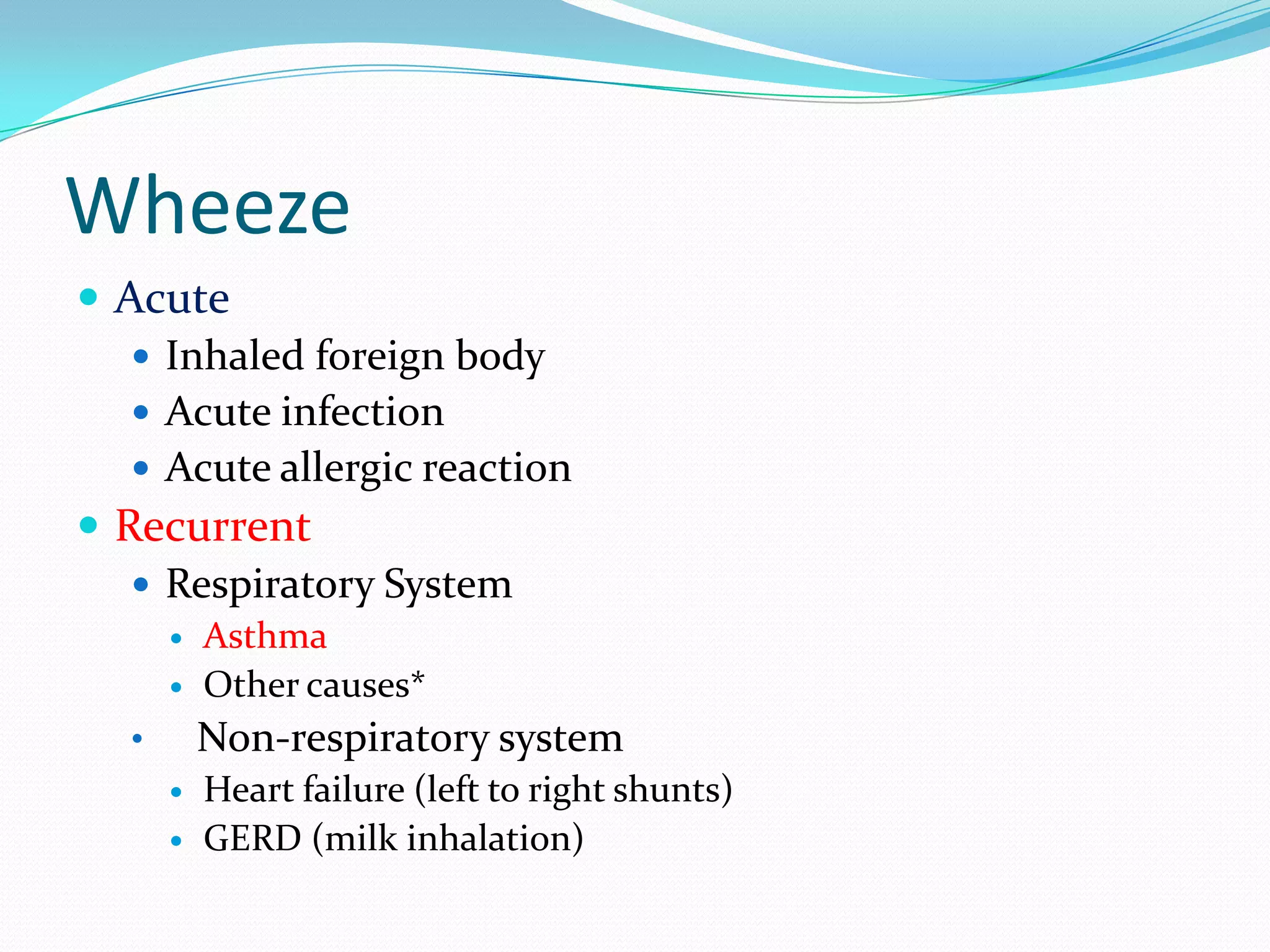
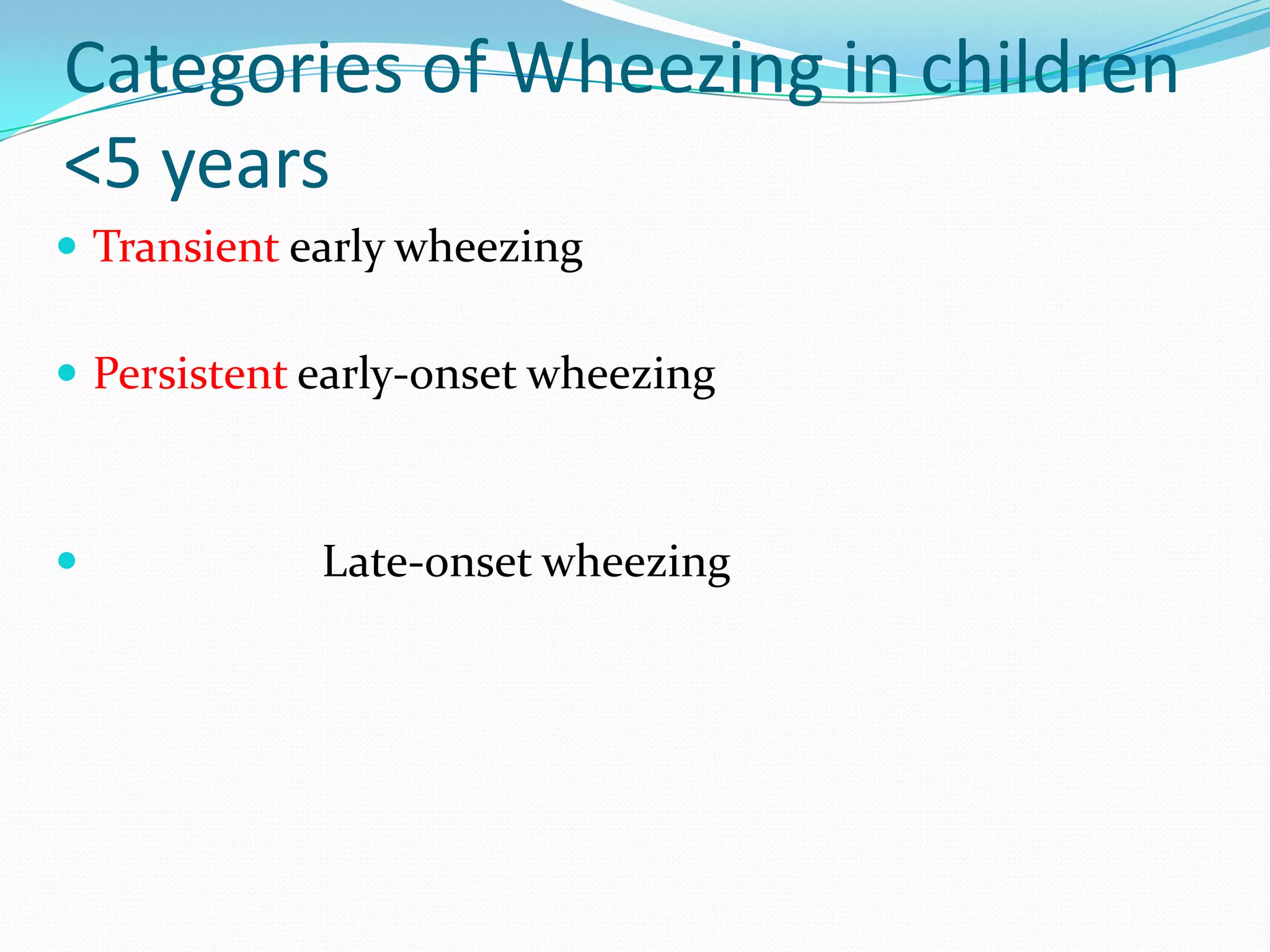
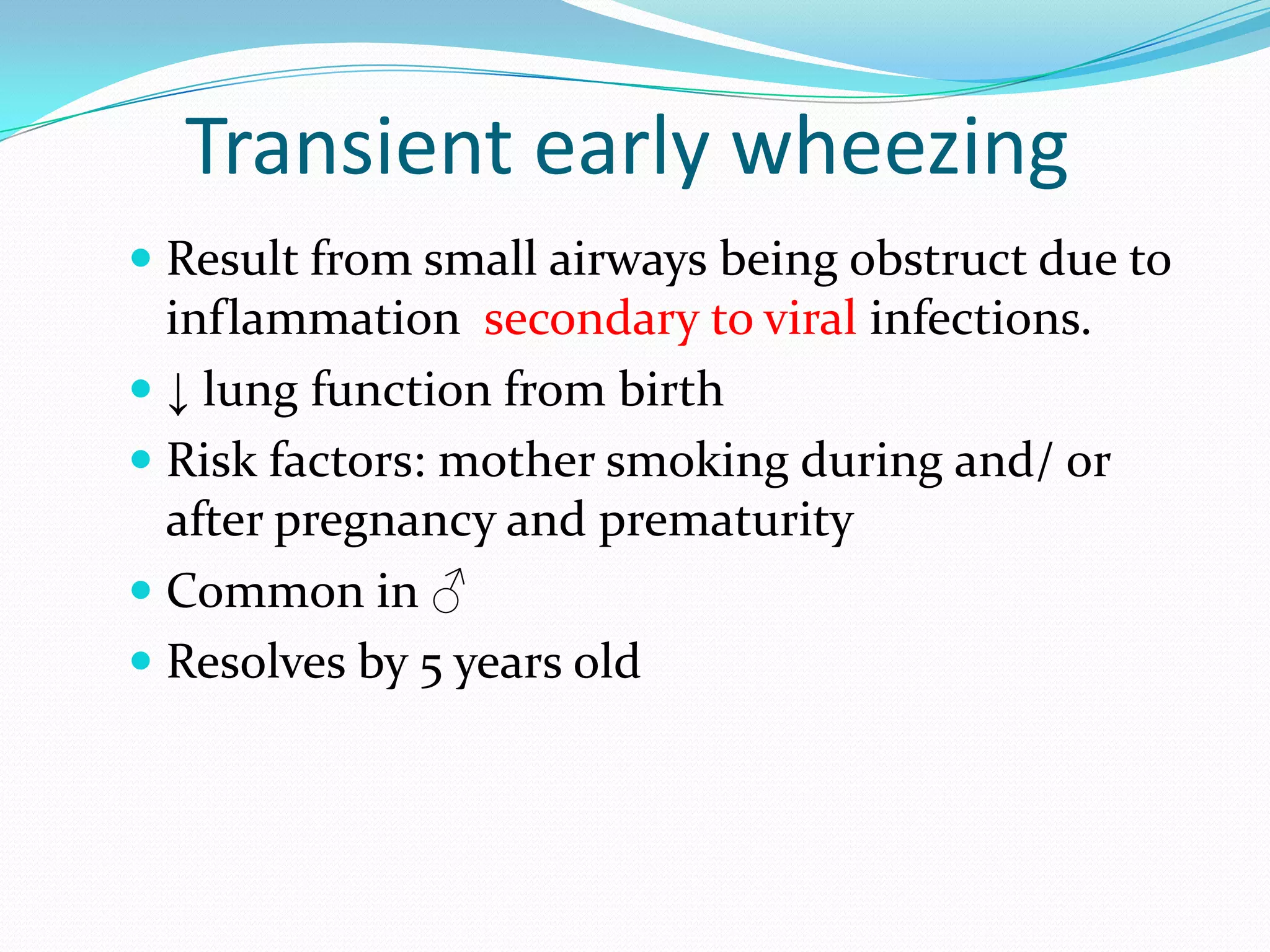
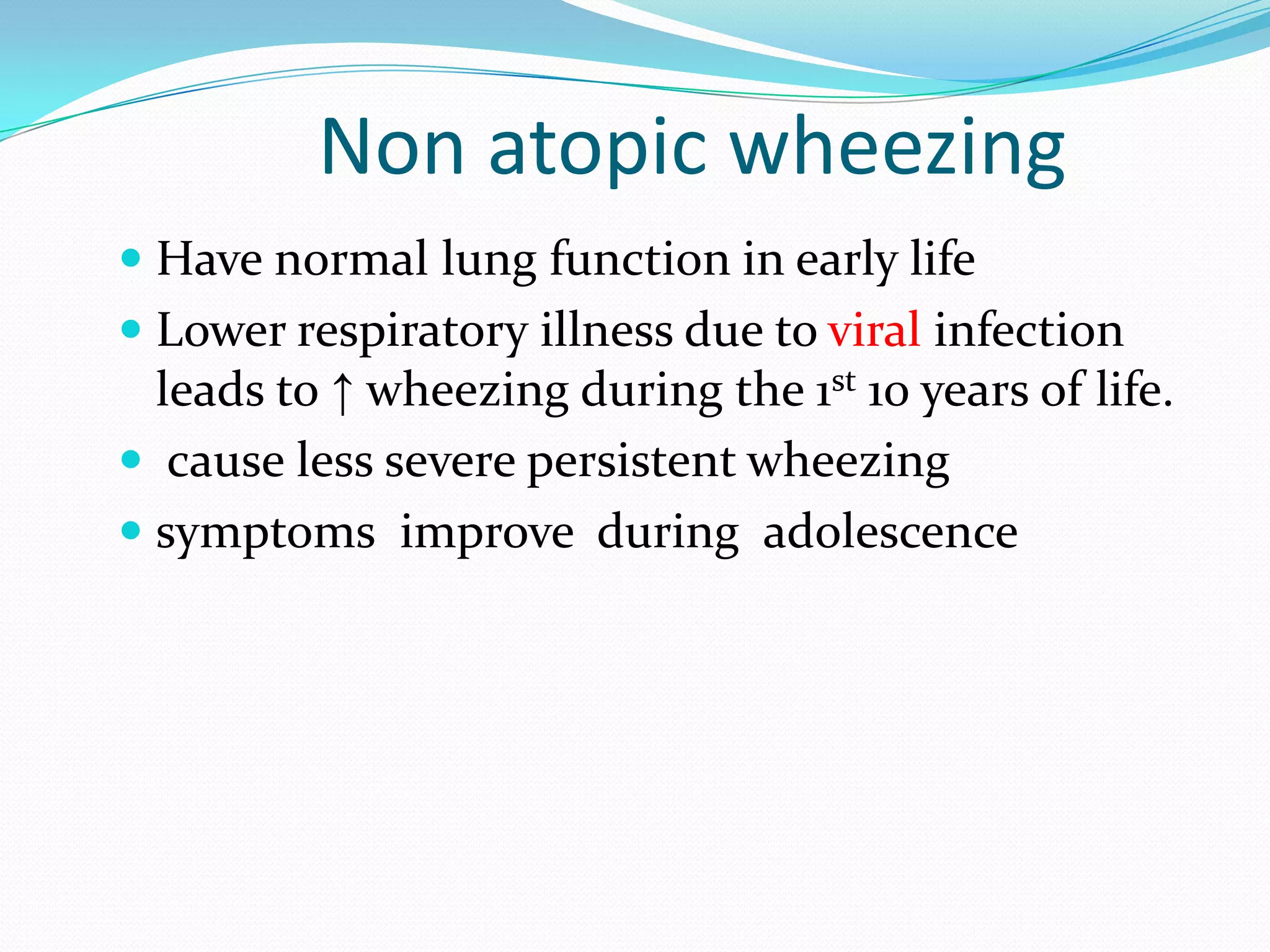
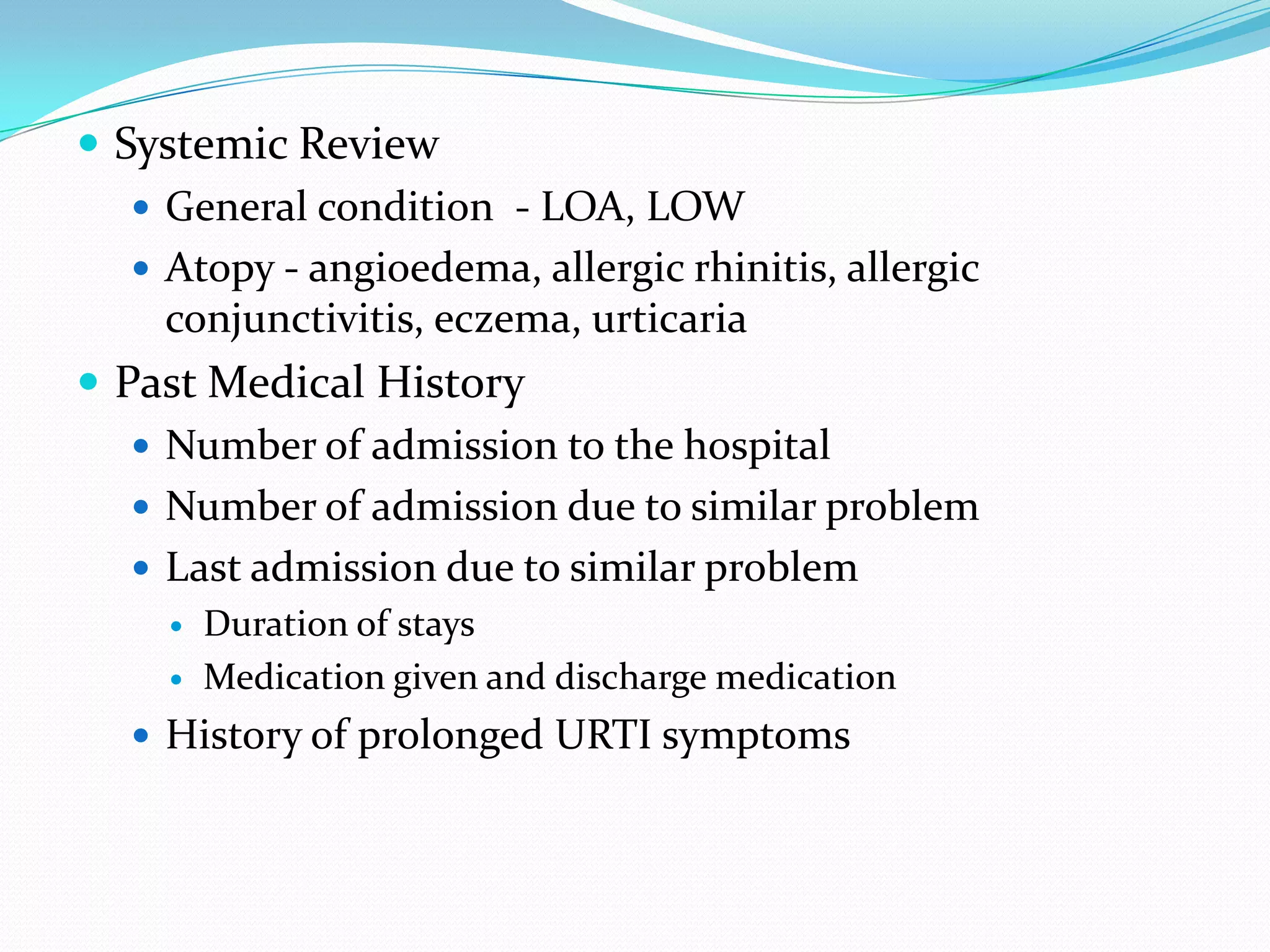
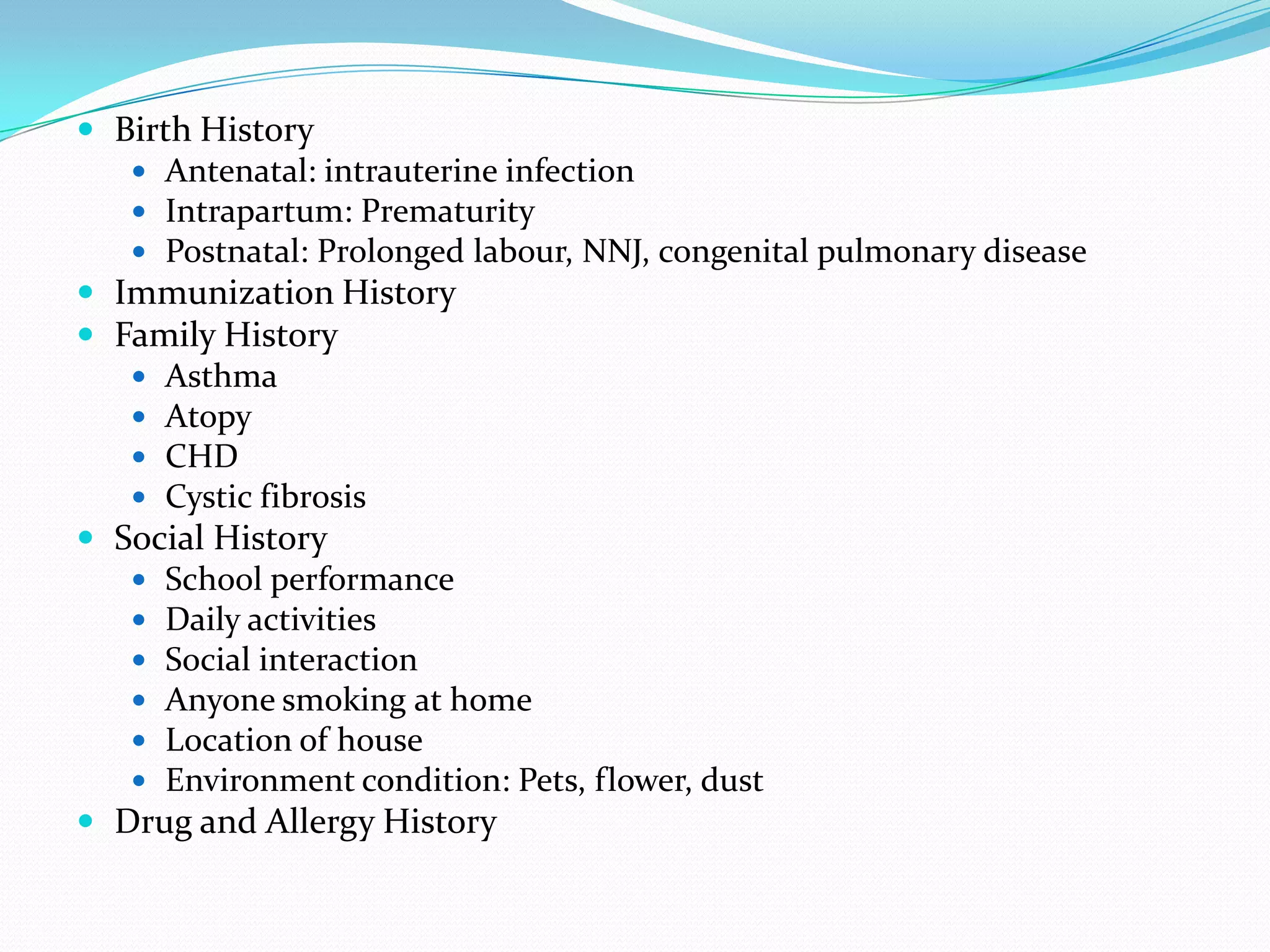
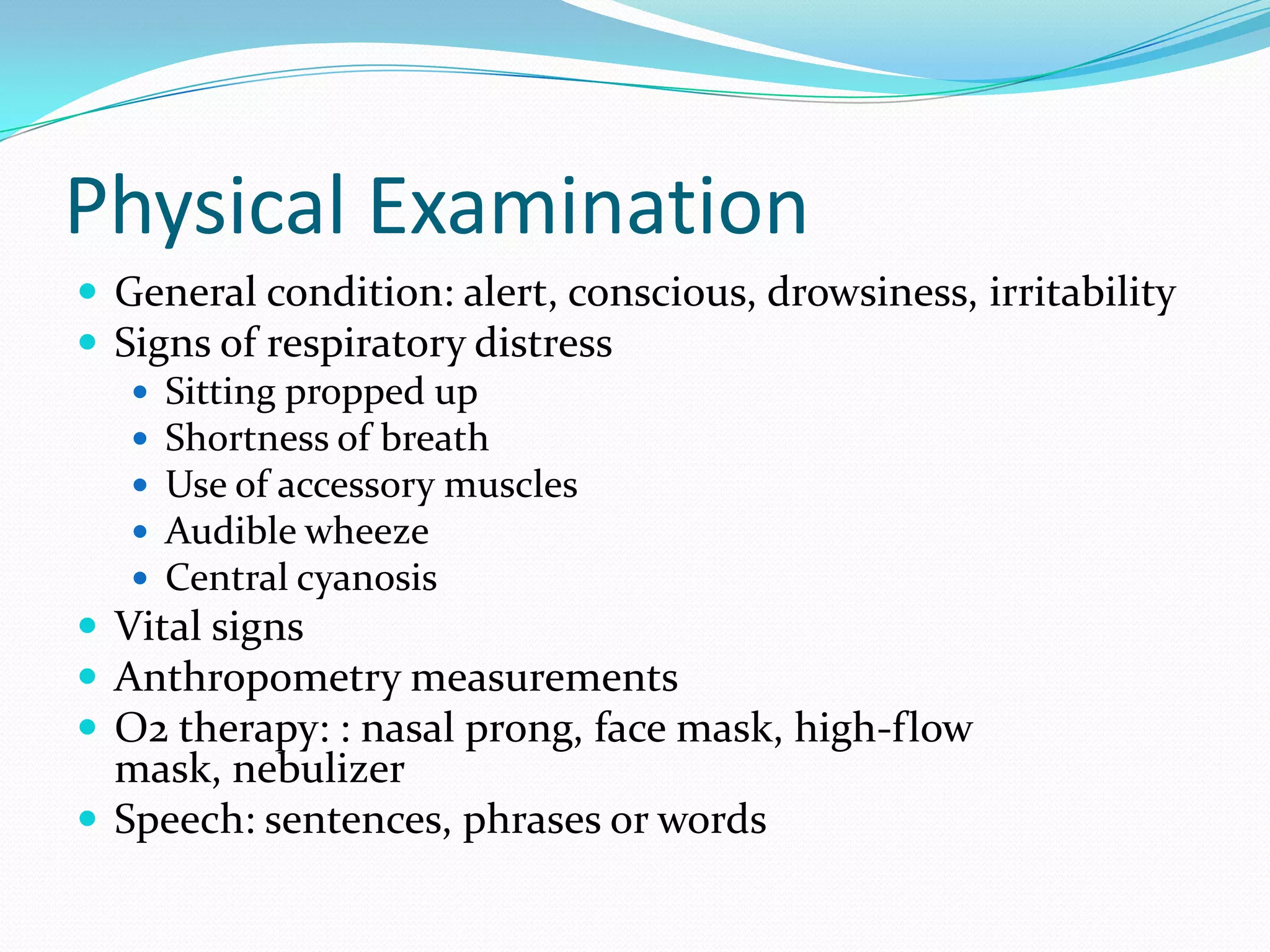
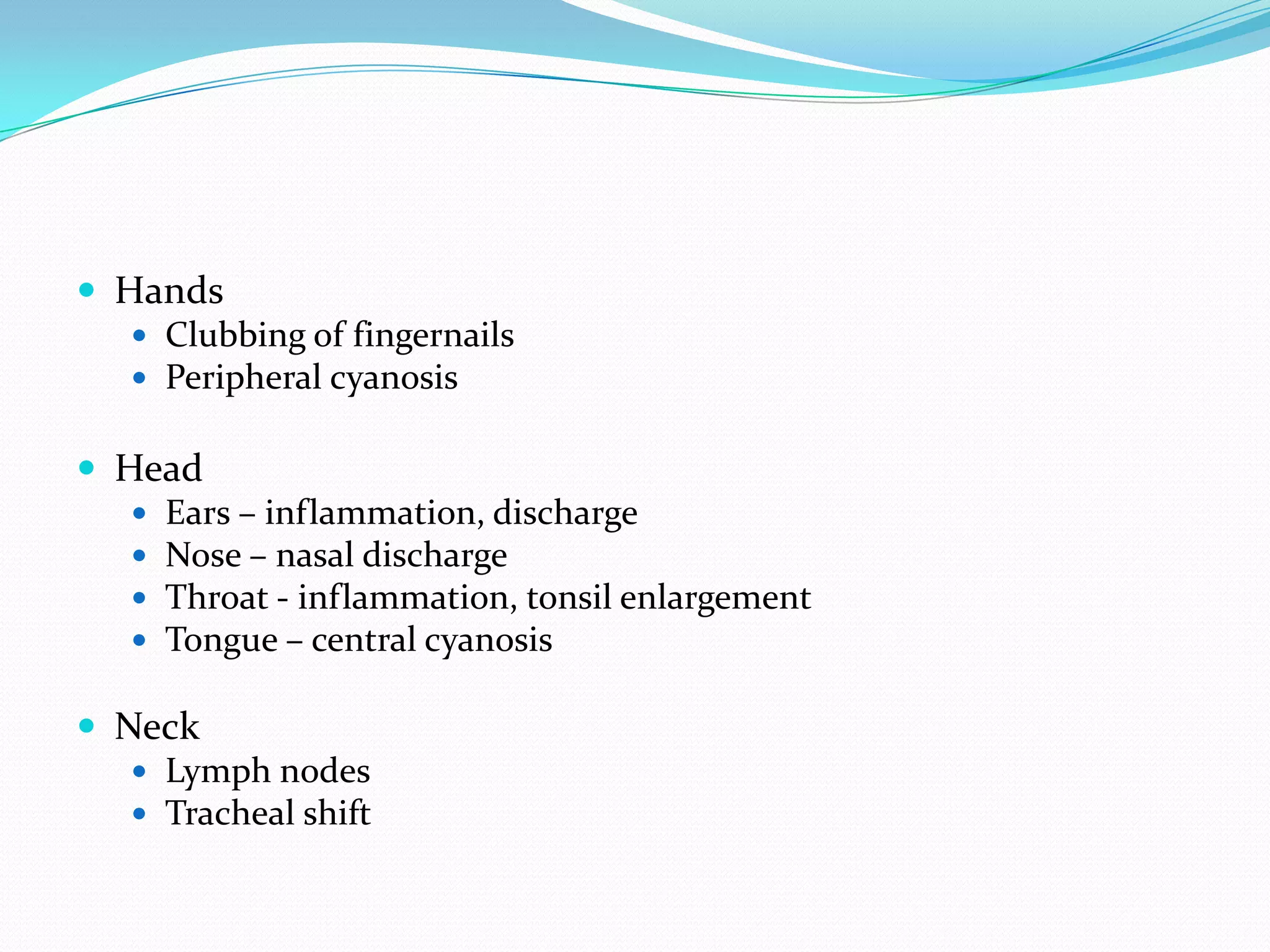
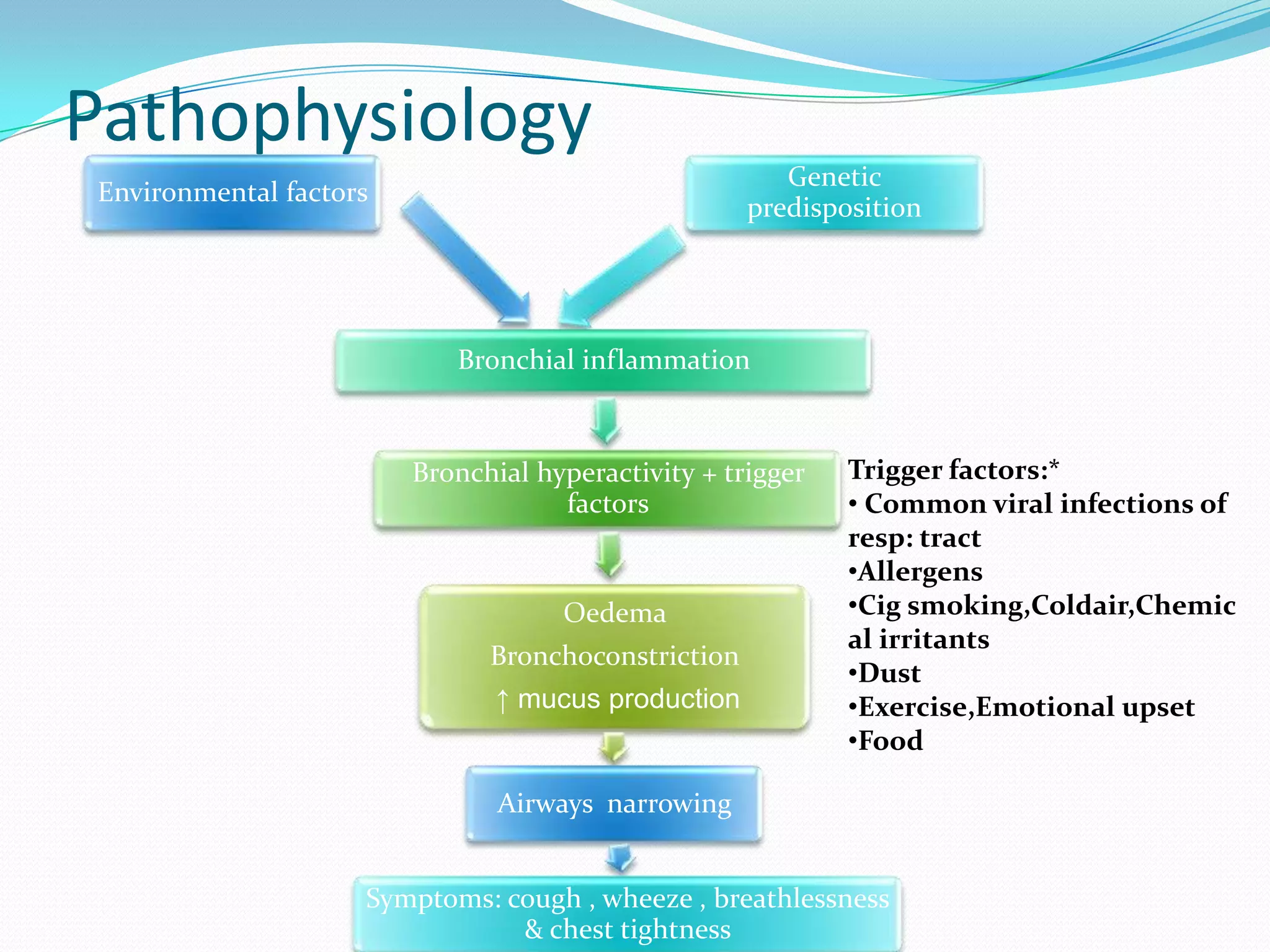
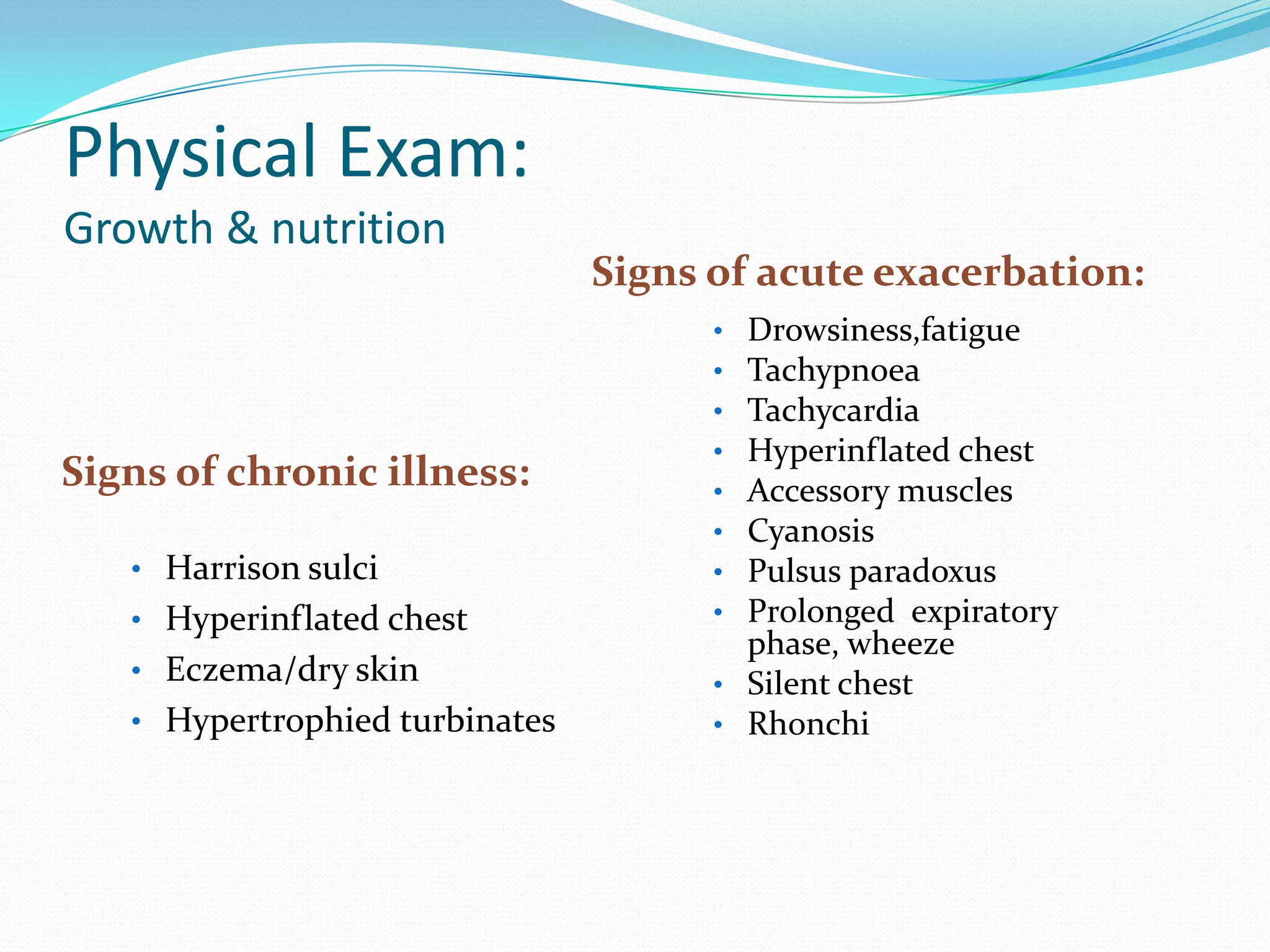
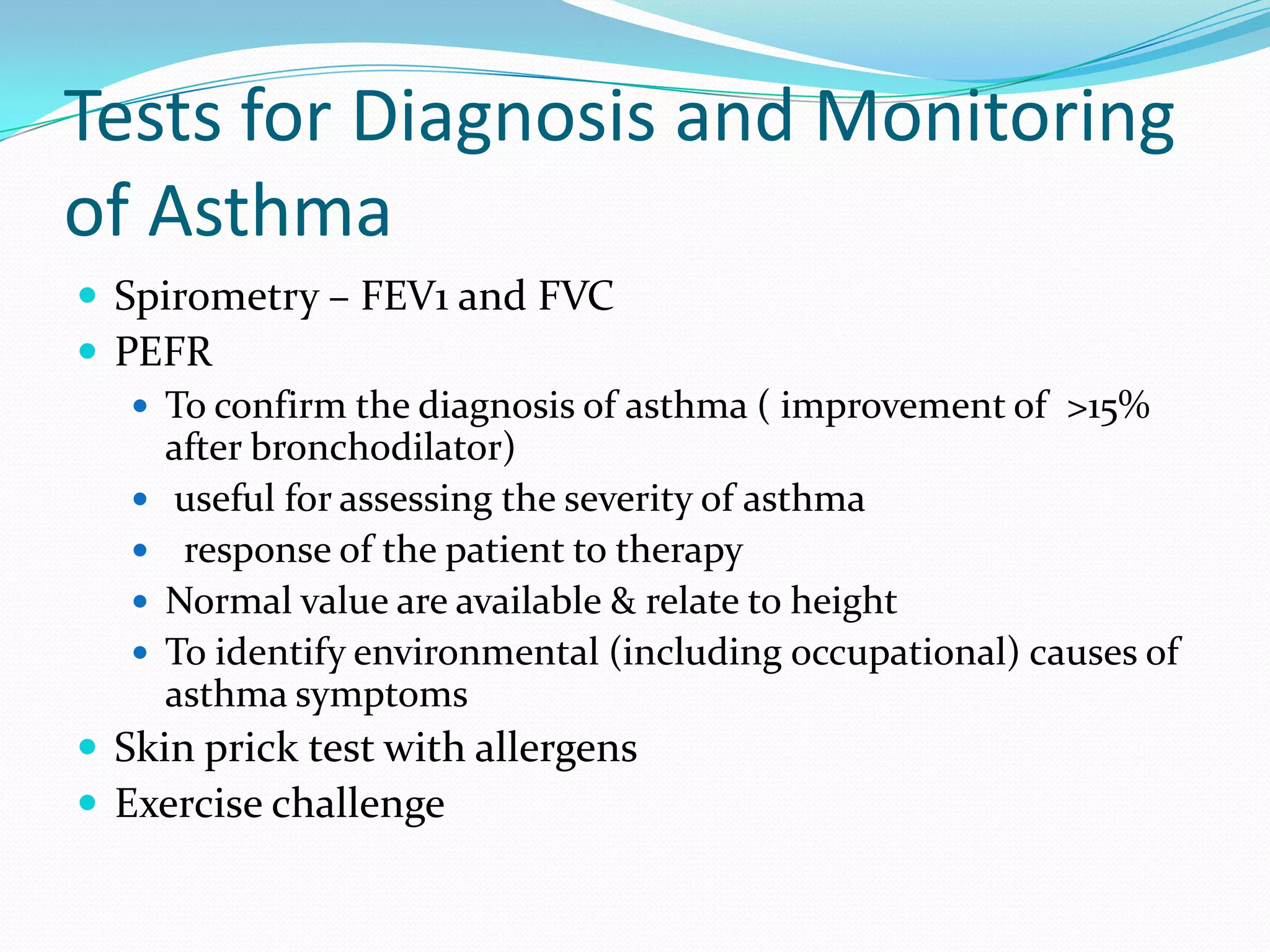
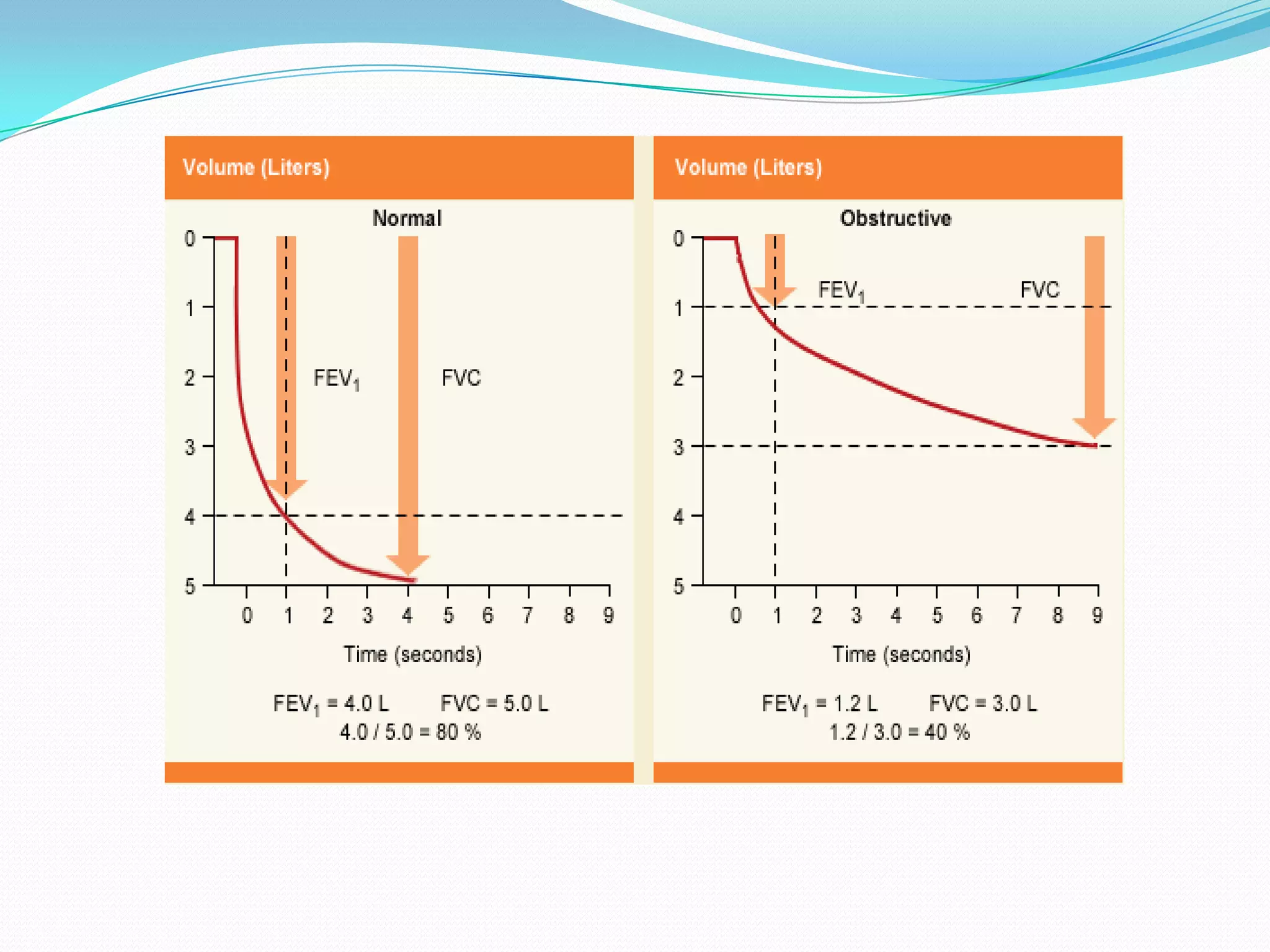
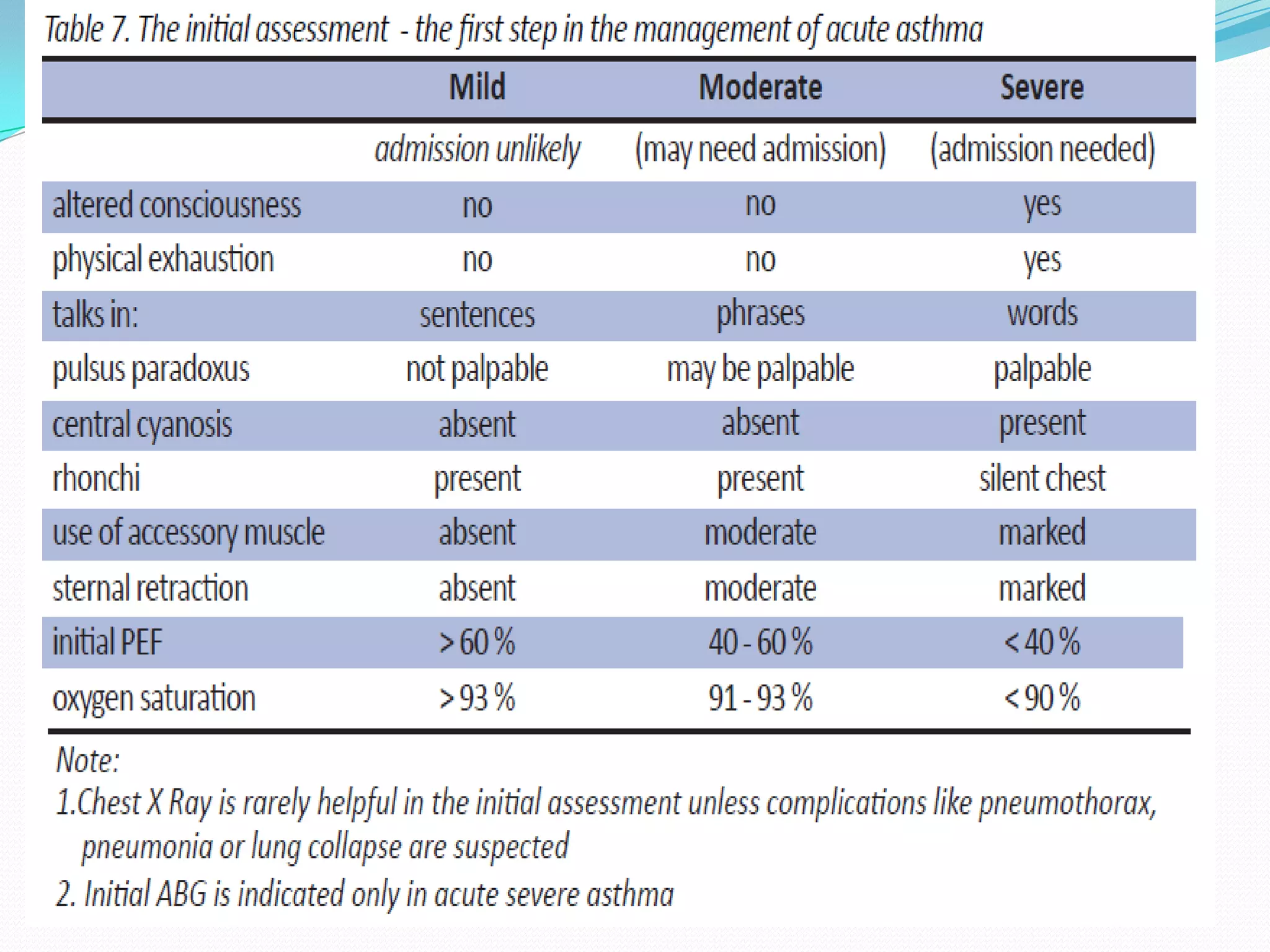
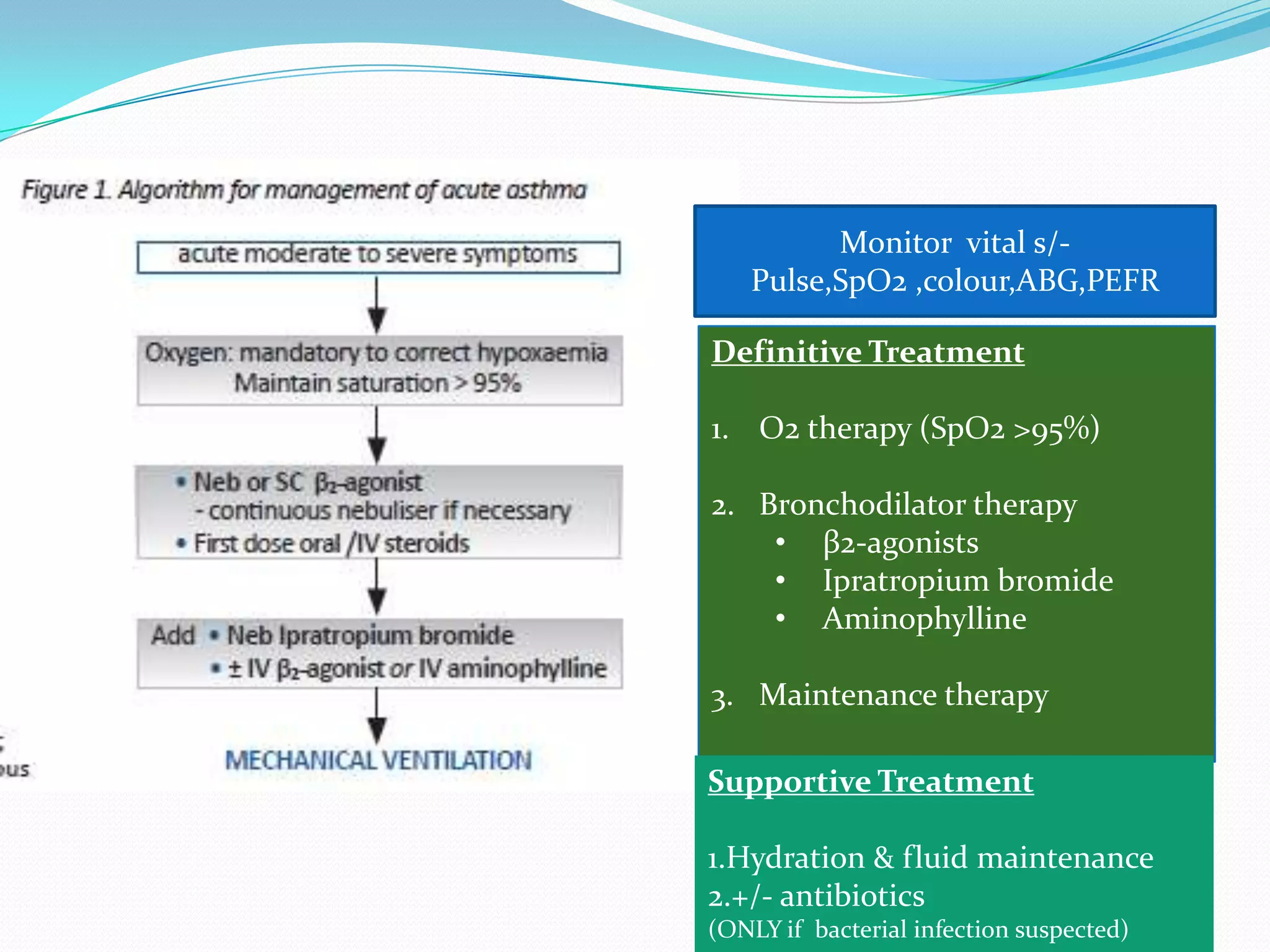
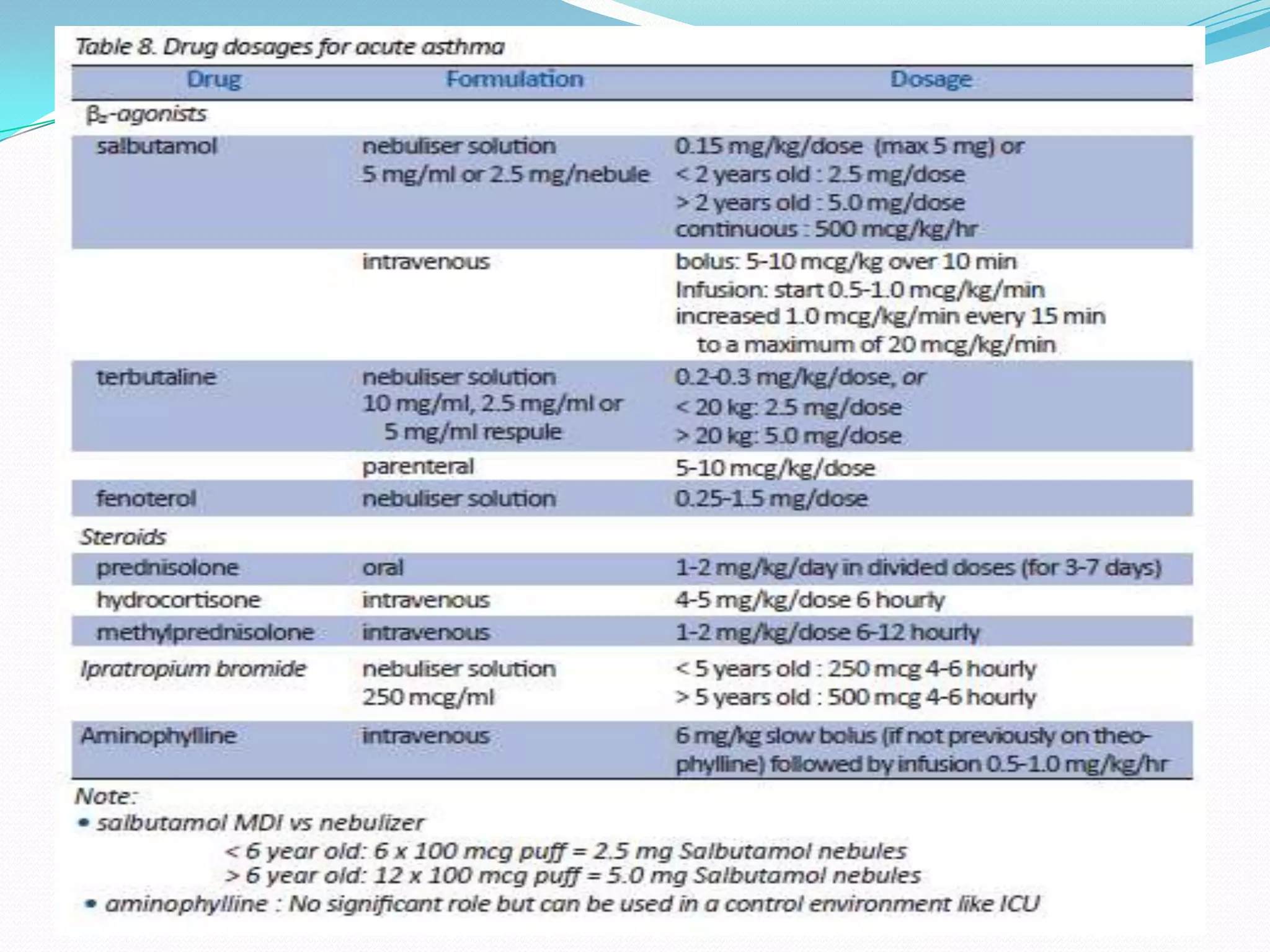
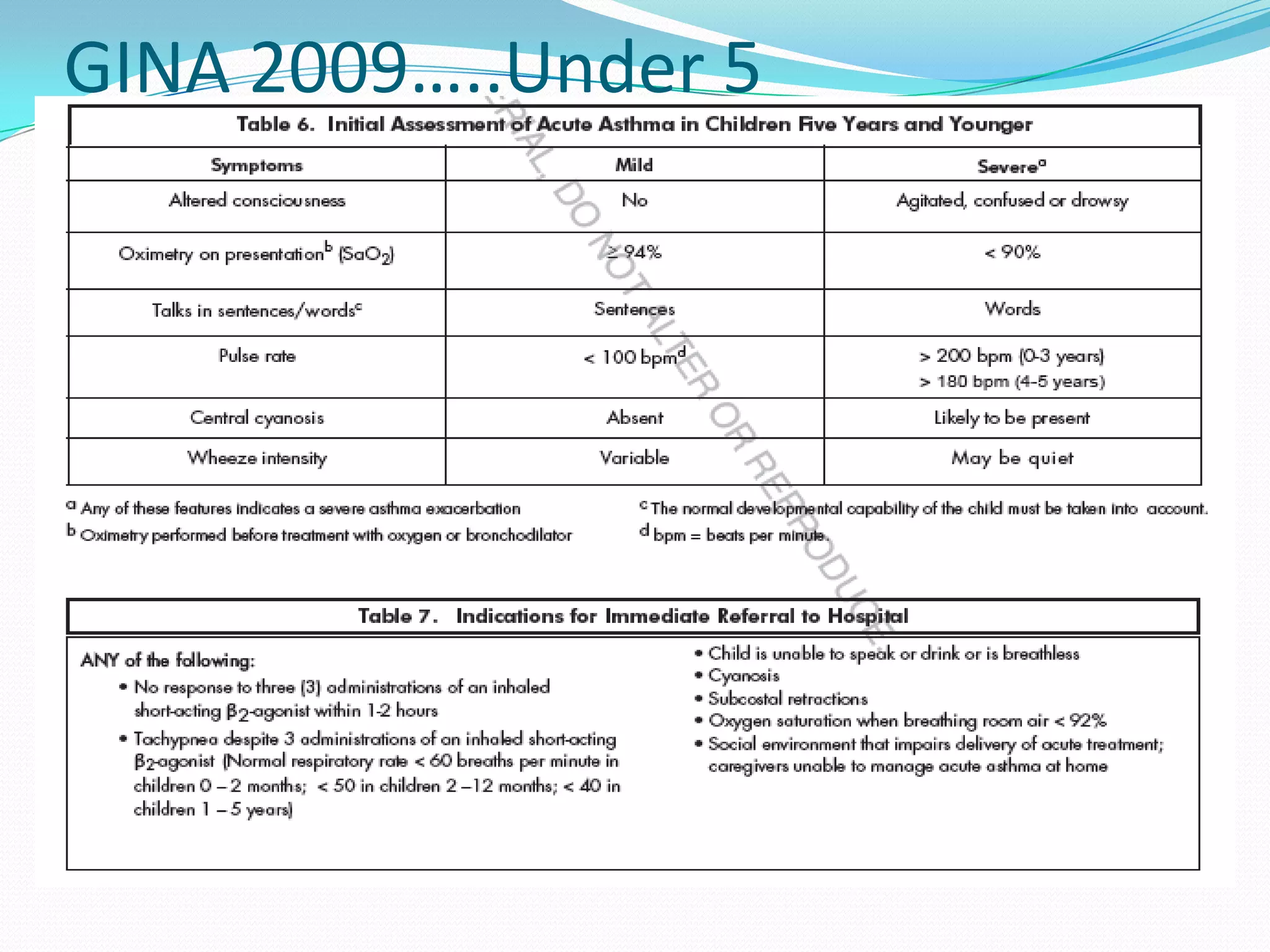
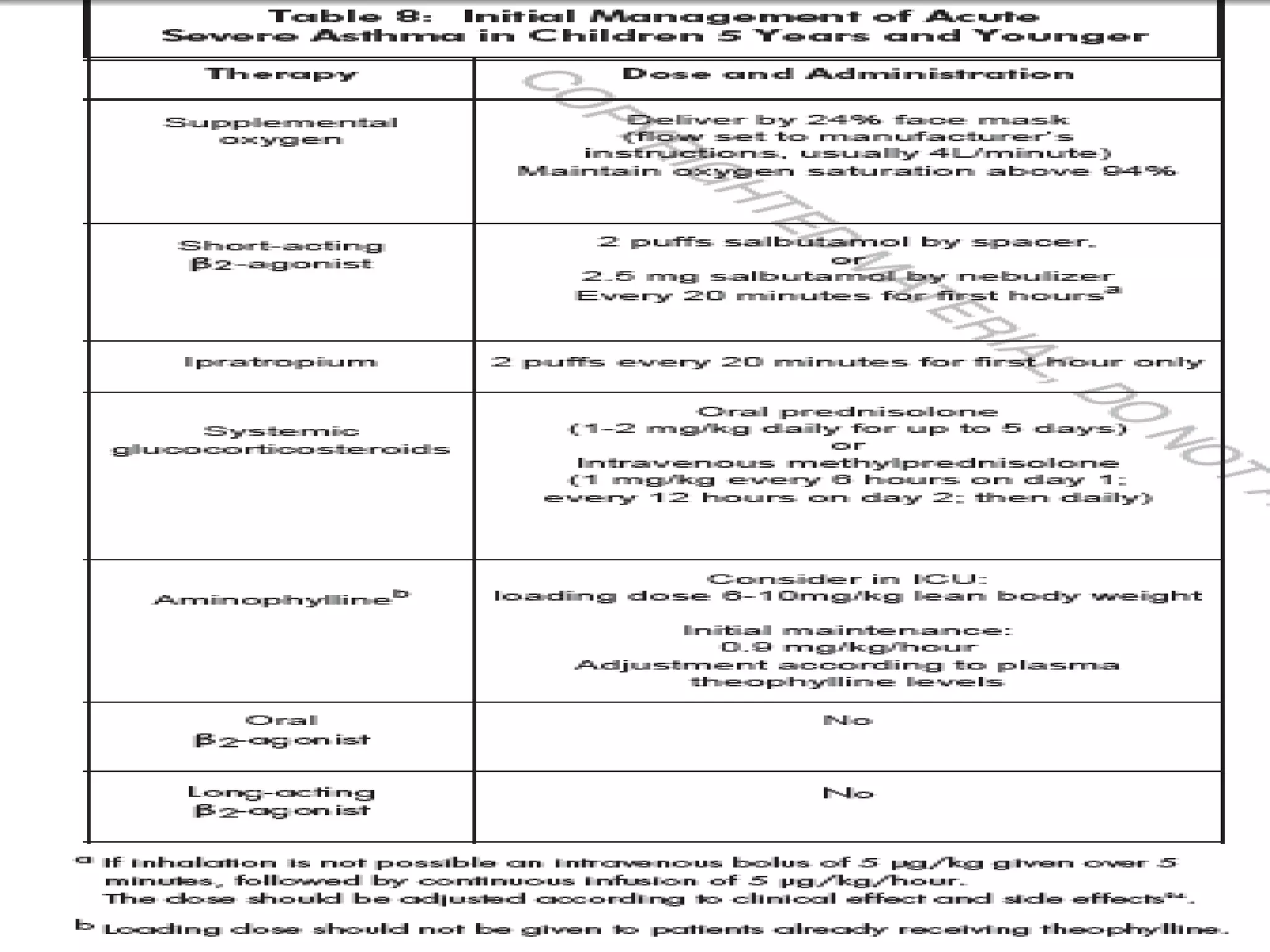
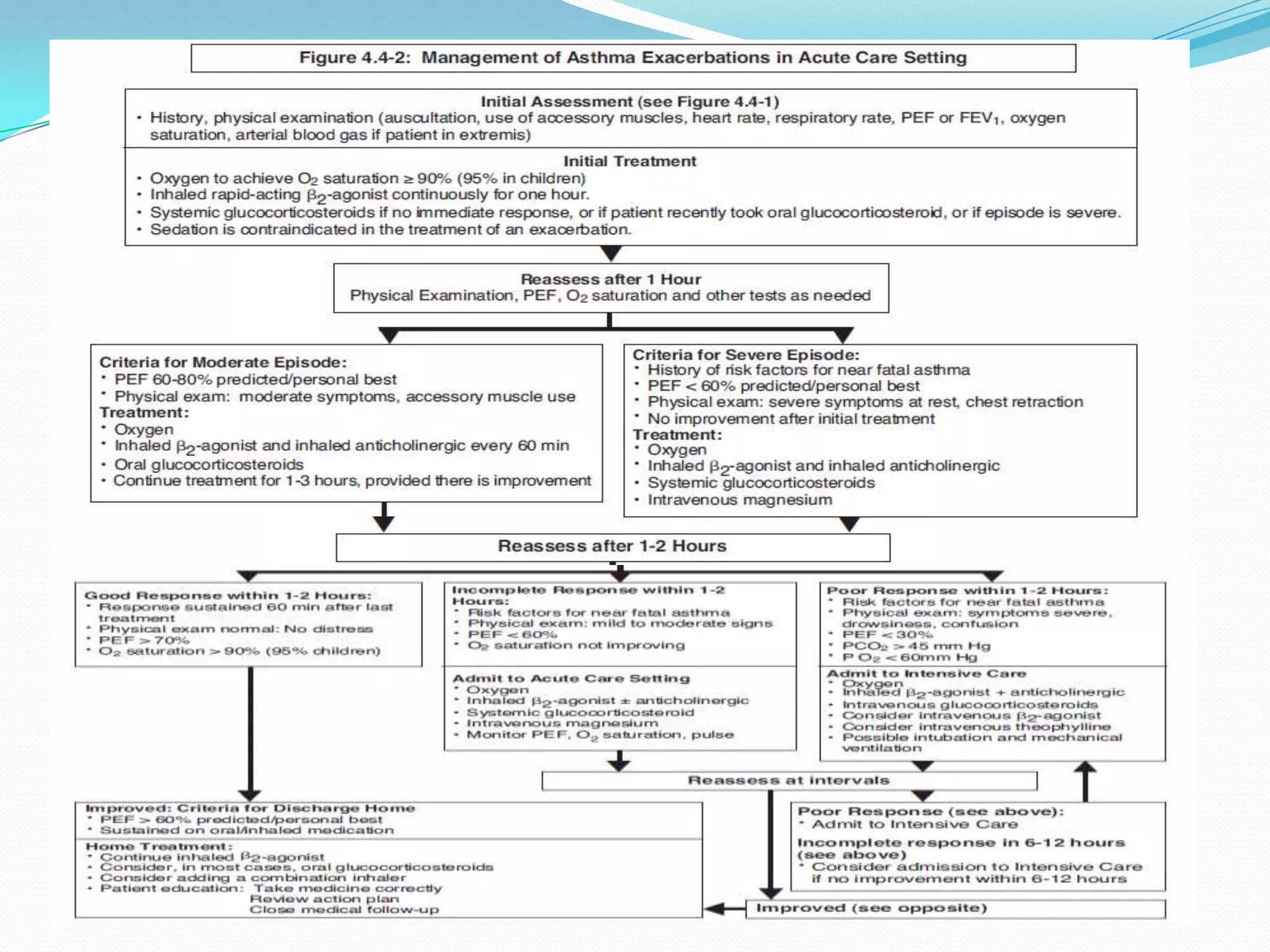
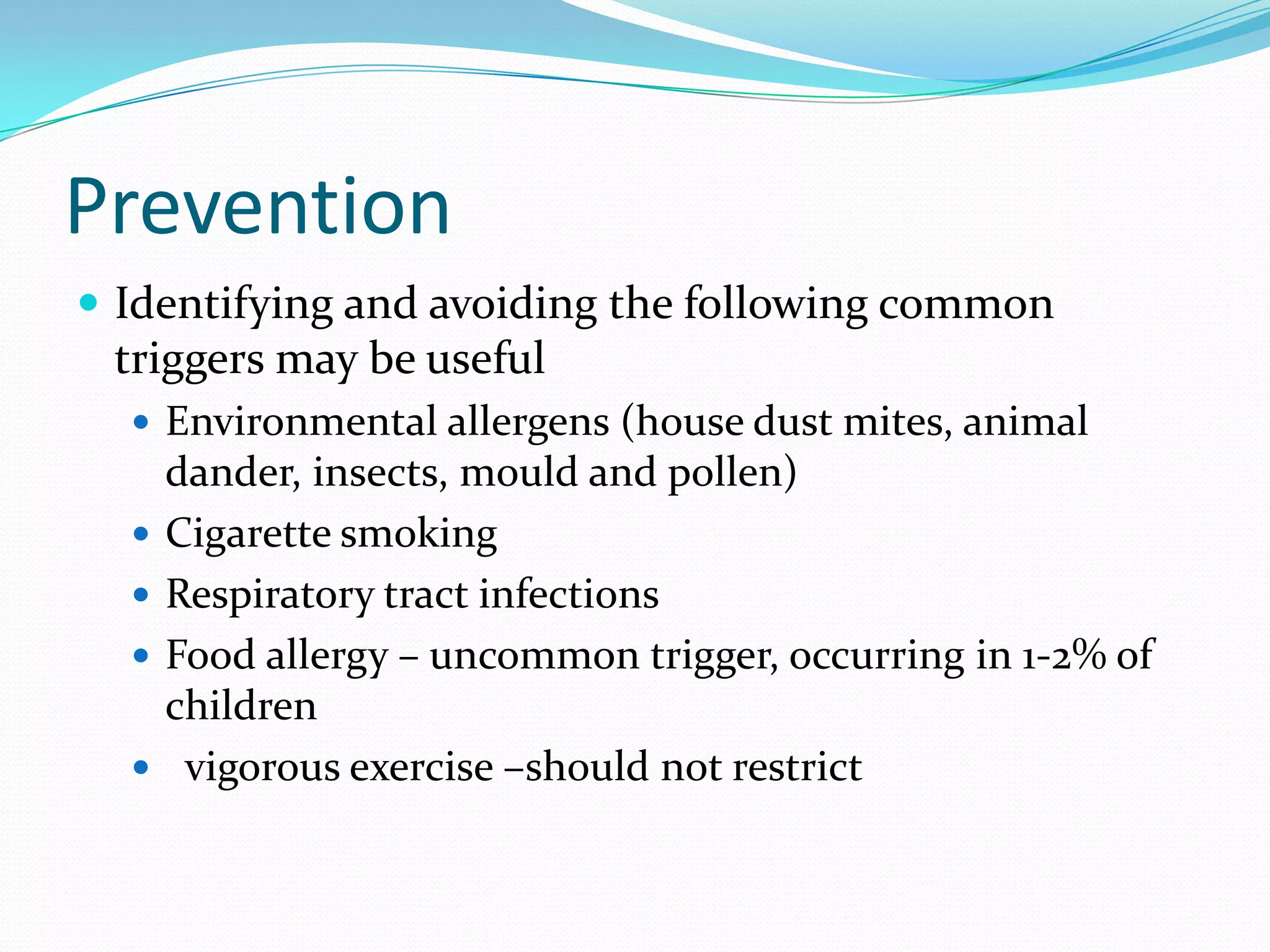
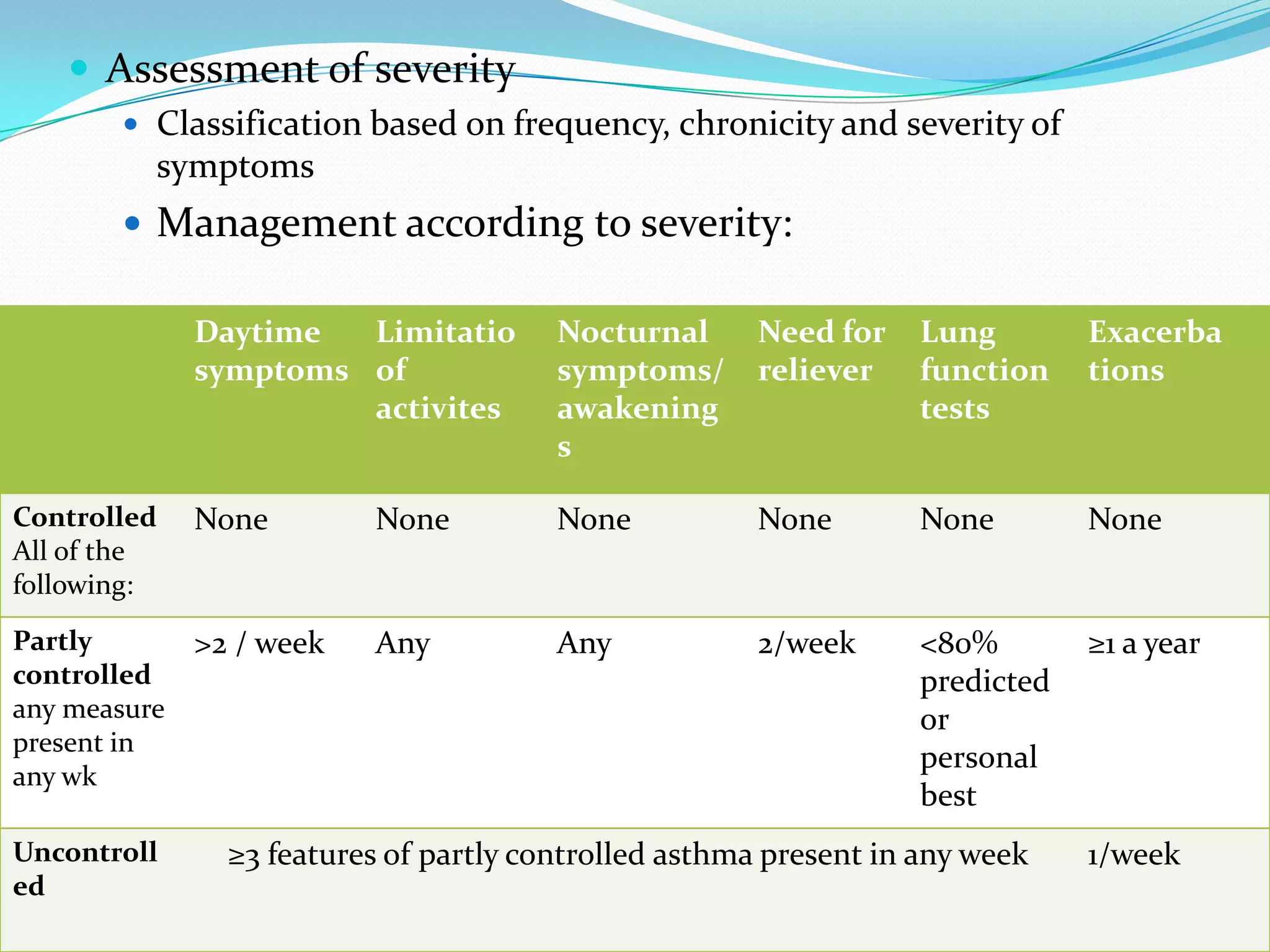
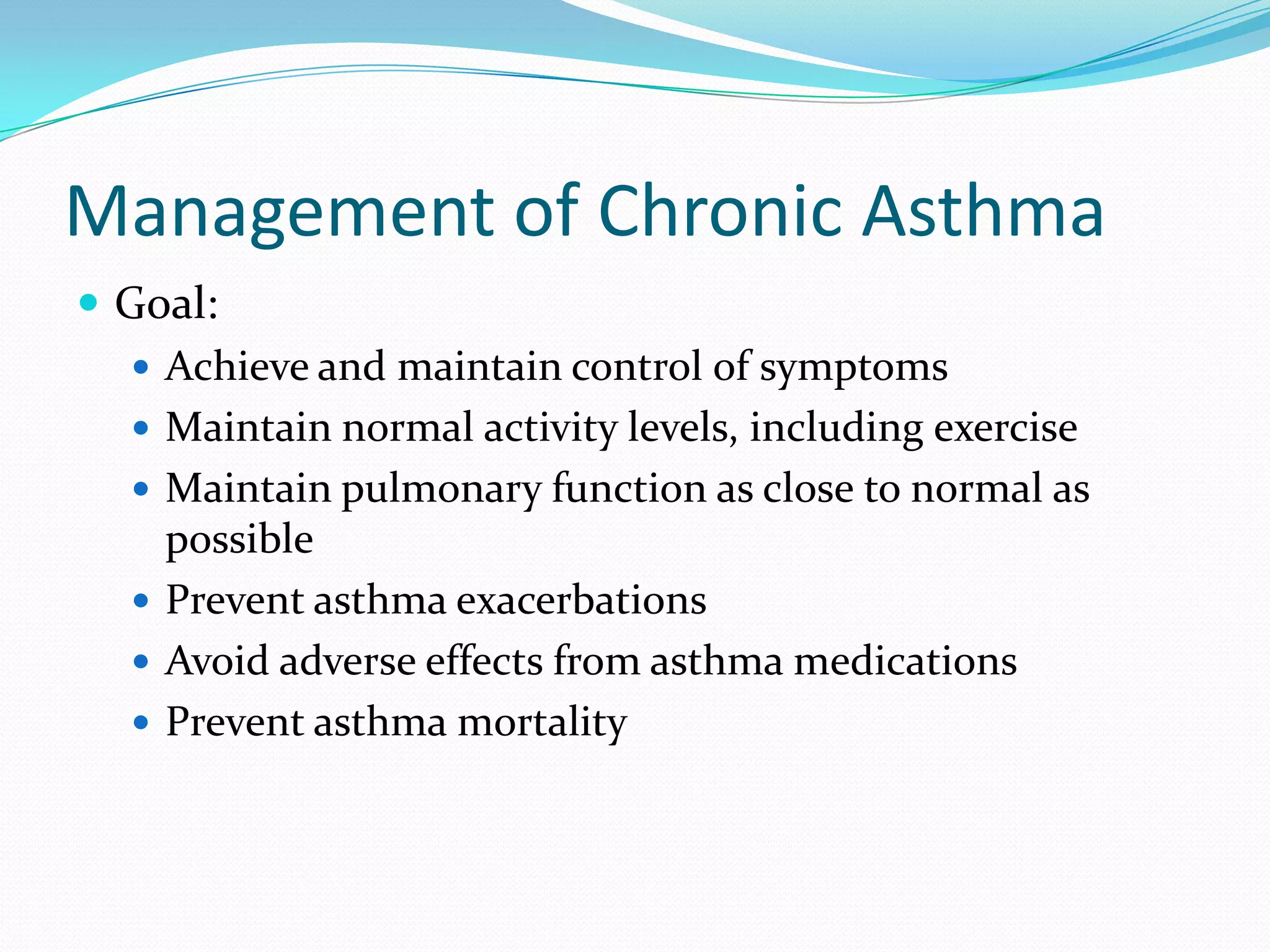
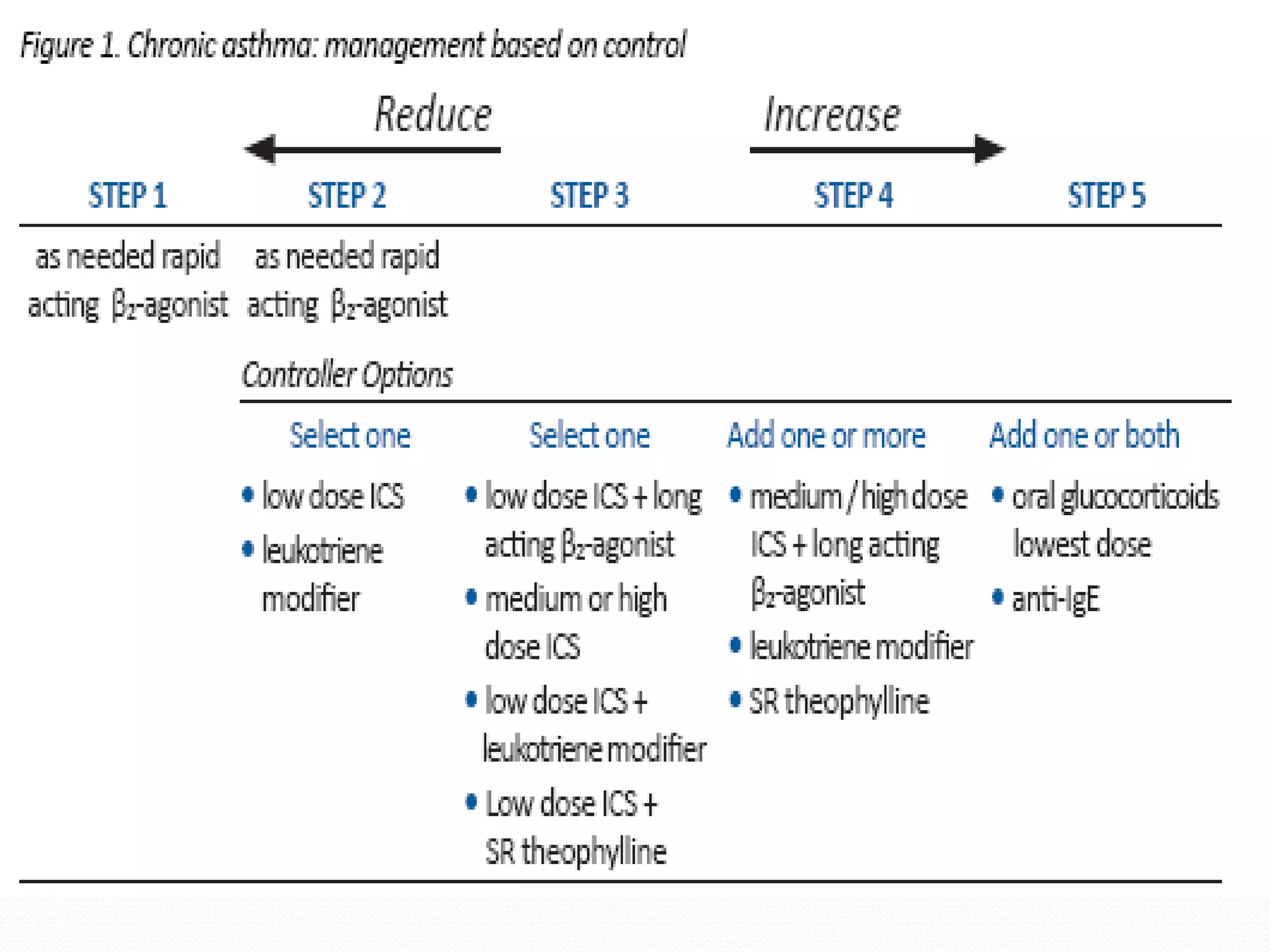
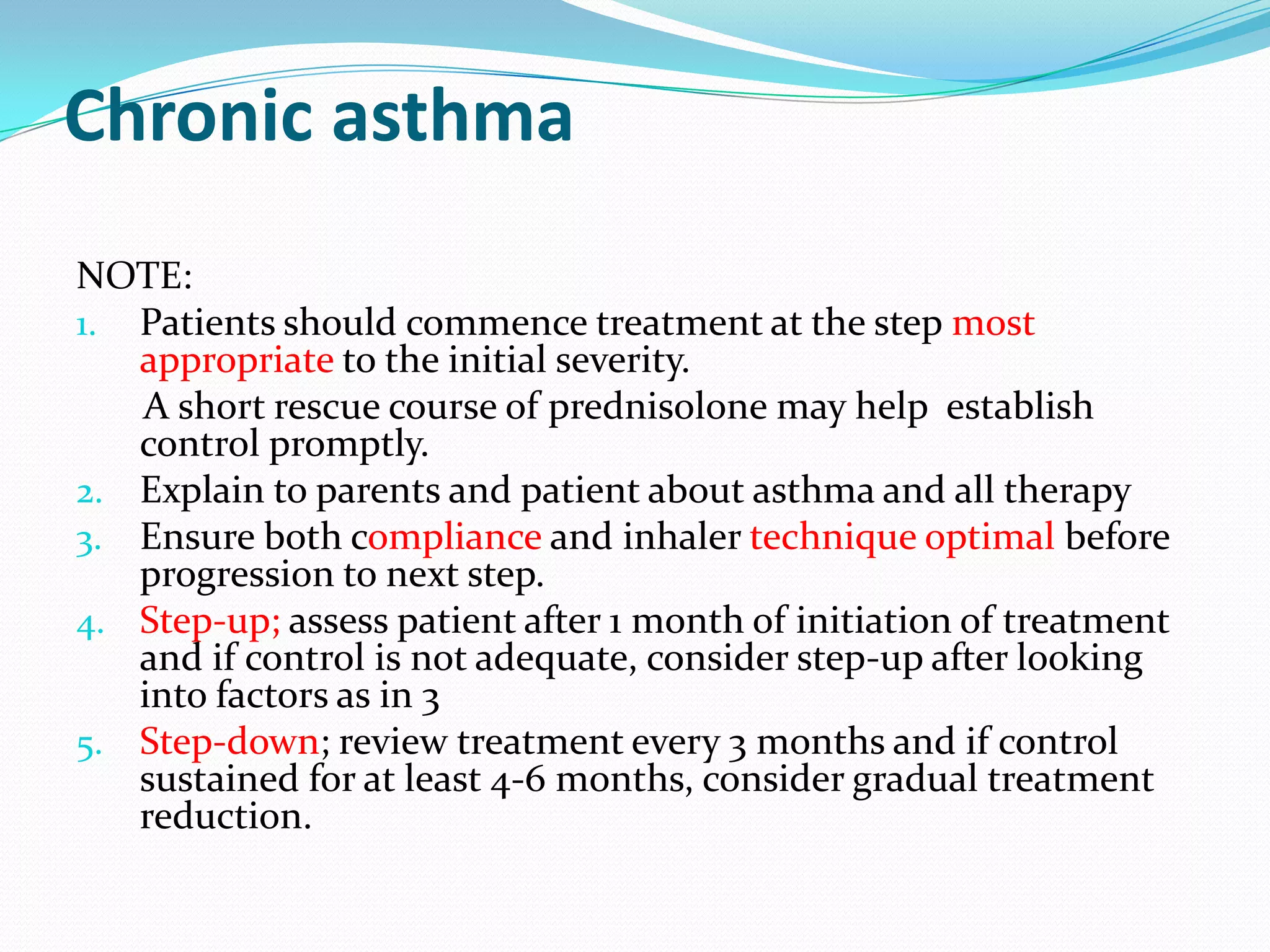
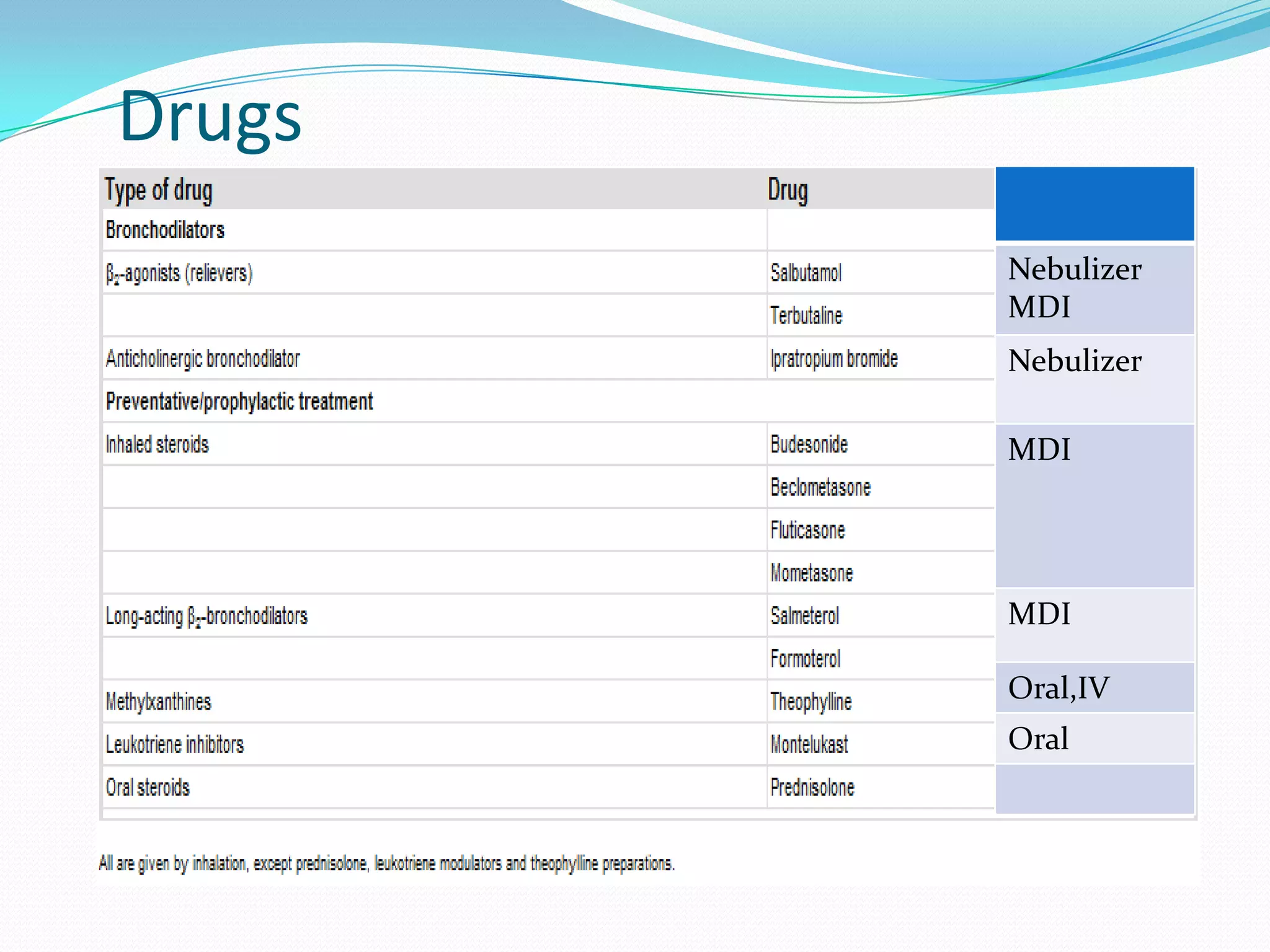
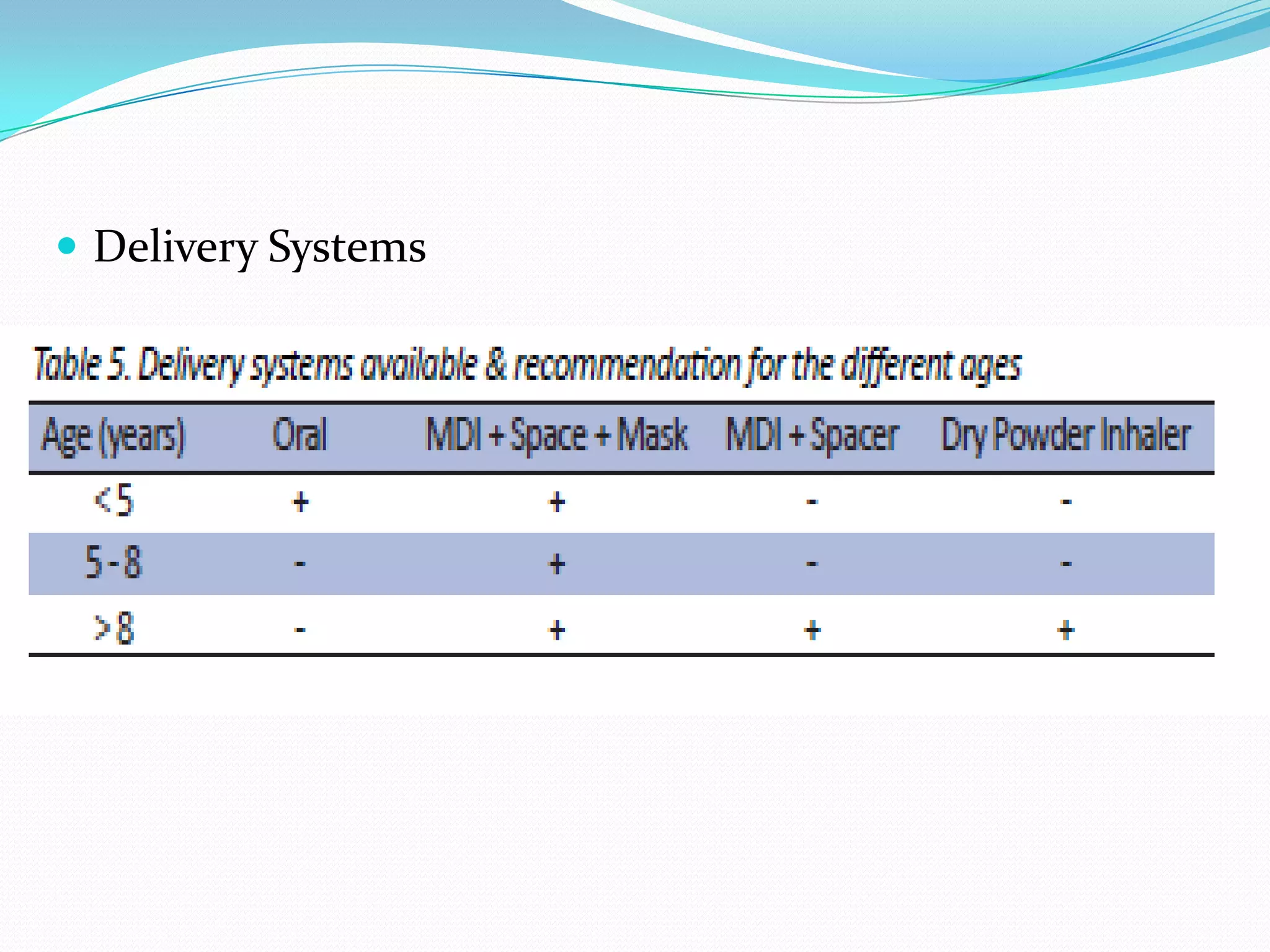
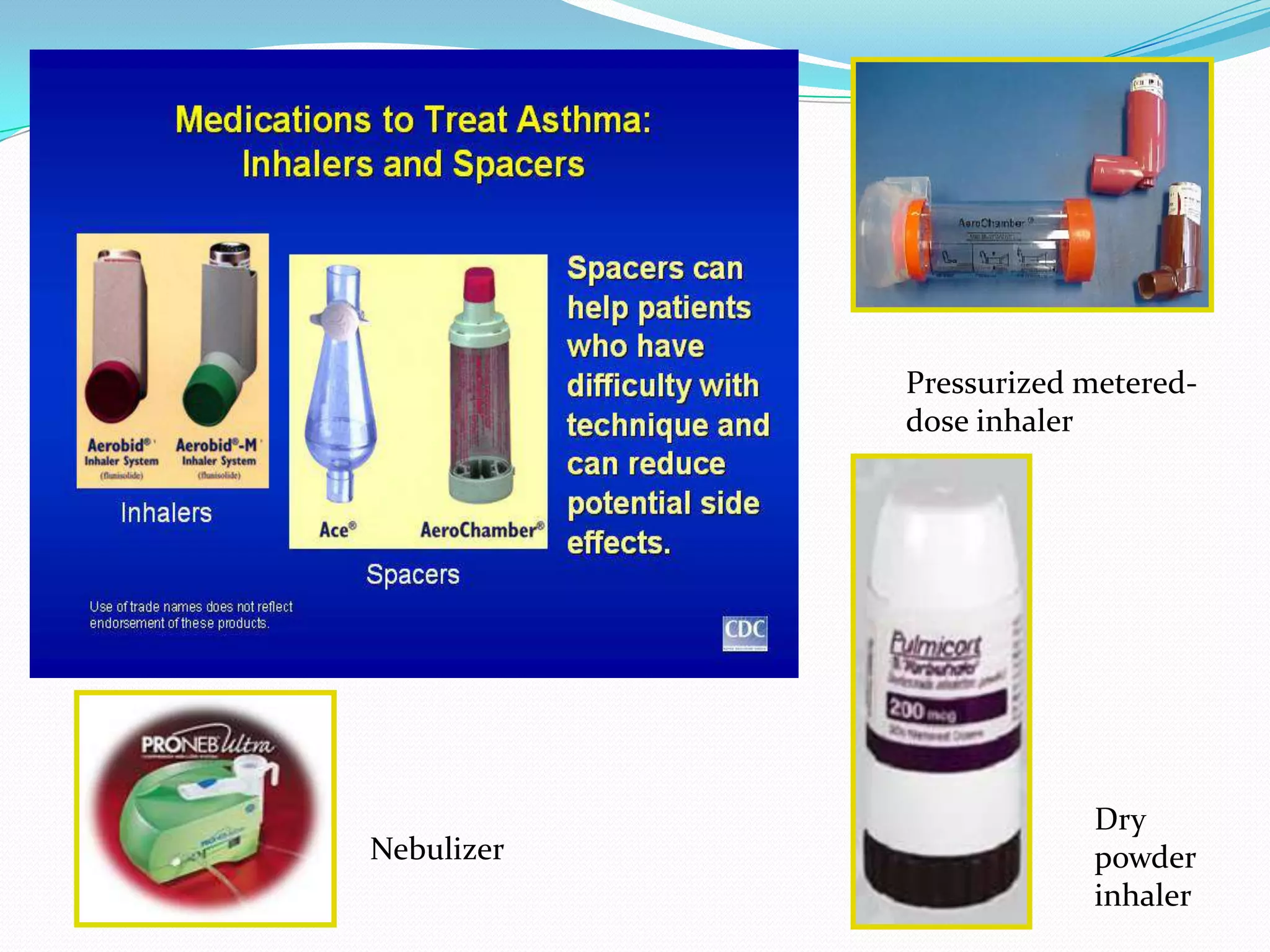
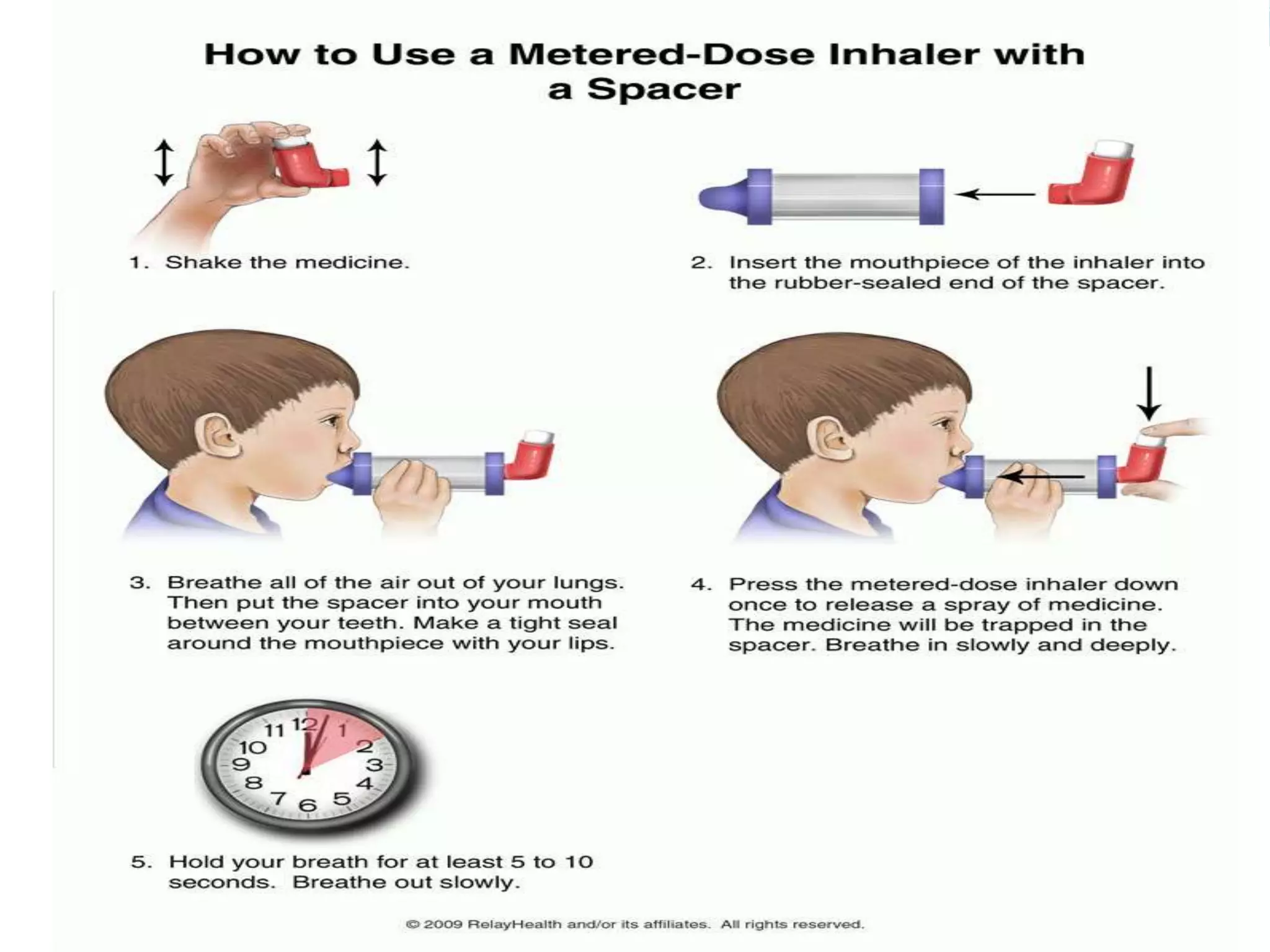
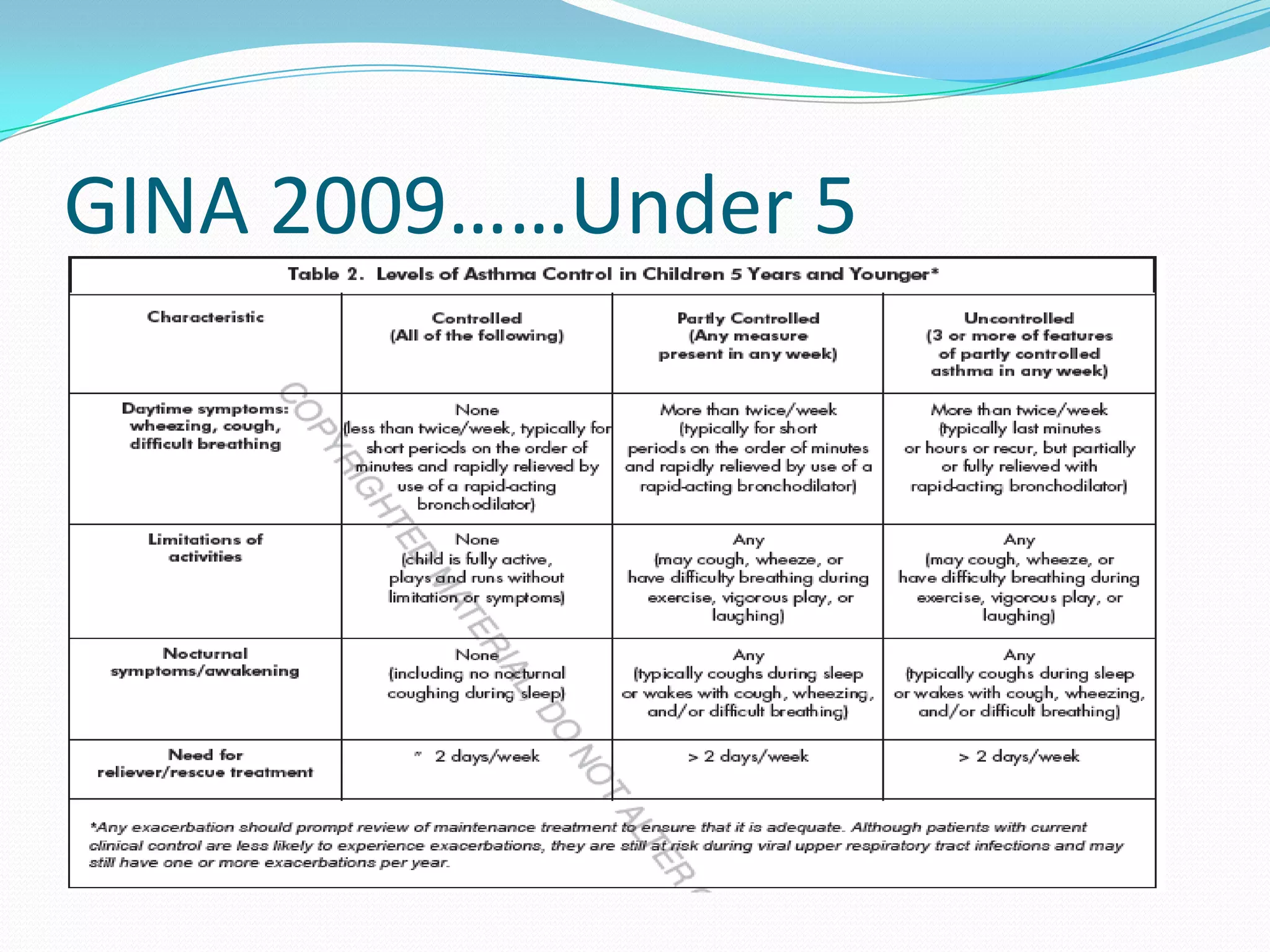
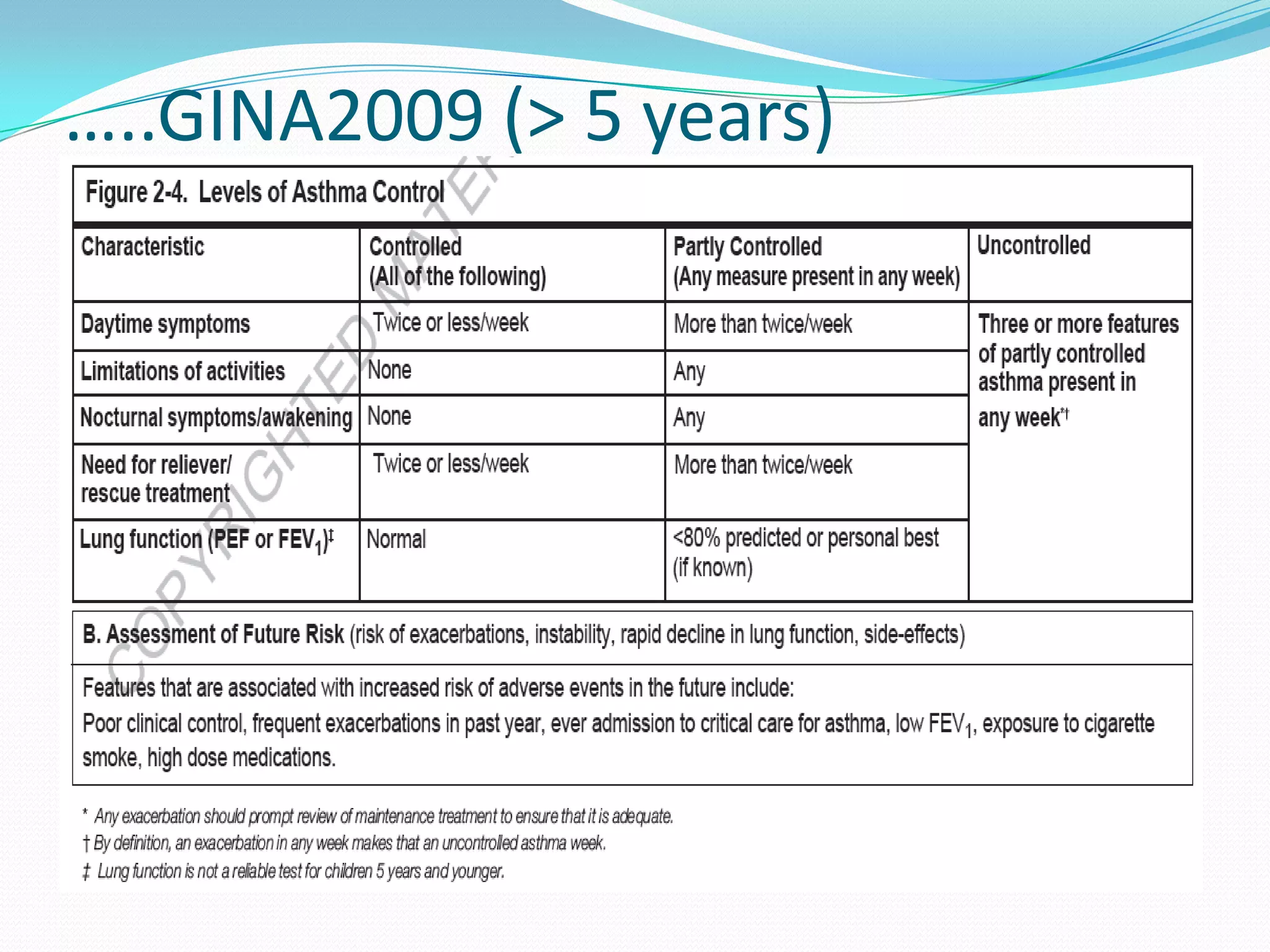
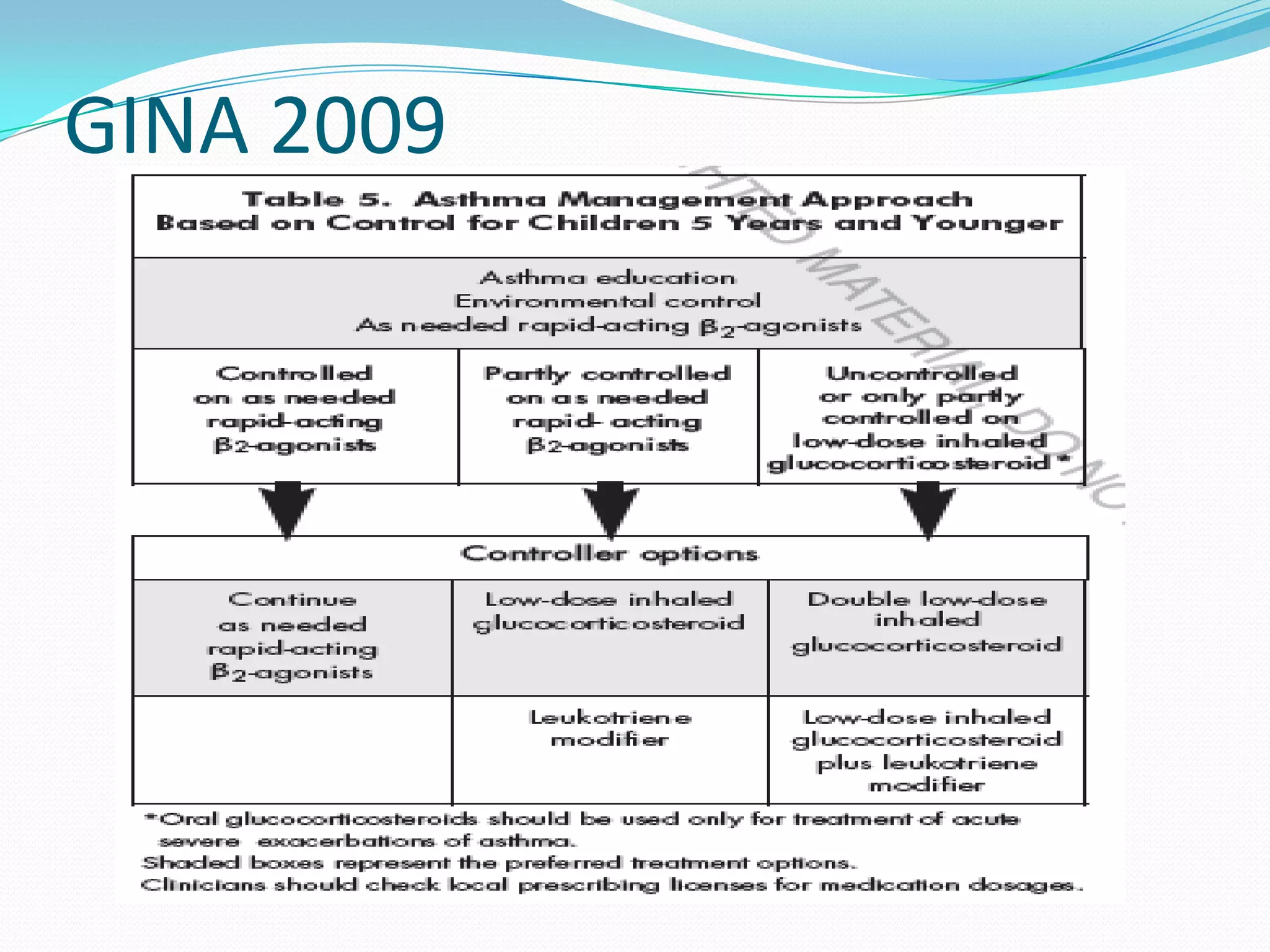
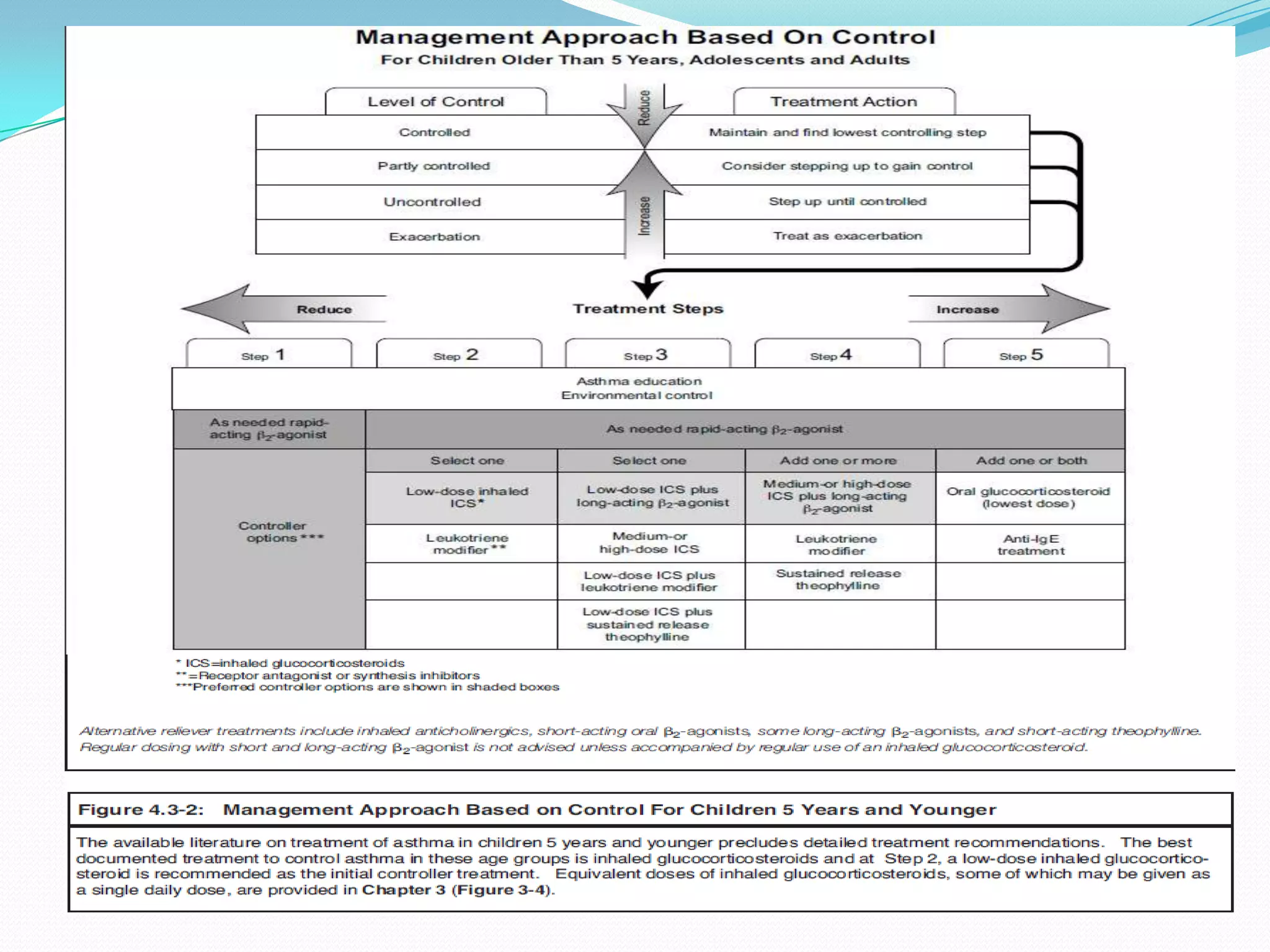
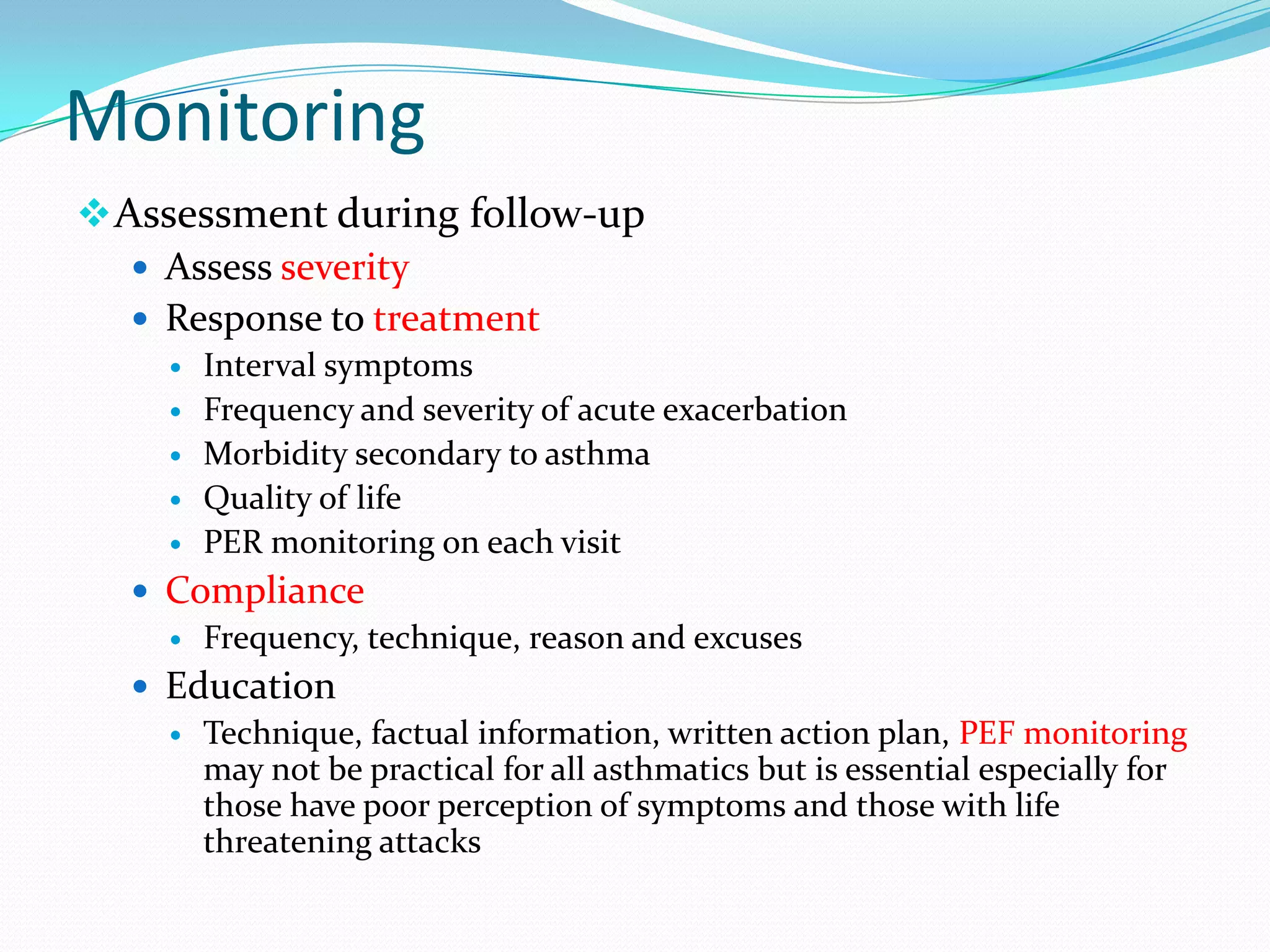
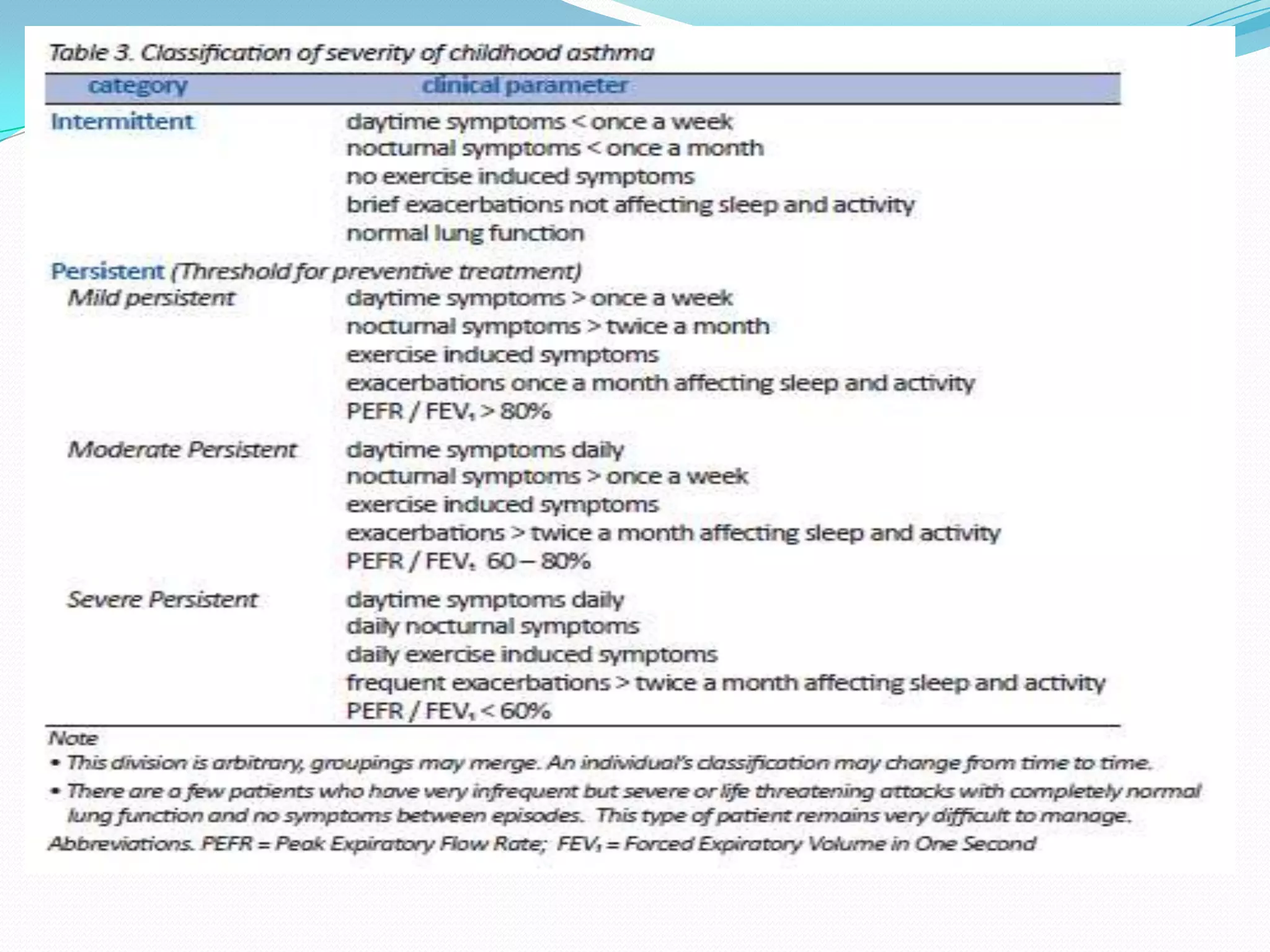
Wheezing is a high-pitched whistling sound produced by narrowed airways during expiration. It is common in children, especially infants and young children under 3 years old. Wheezing can be acute due to infections or allergies, or recurrent due to conditions like asthma. Asthma is a chronic inflammatory airway disease characterized by wheezing, coughing, and breathlessness. Risk factors include family history of atopy and exposure to cigarette smoke. Diagnosis involves assessing symptoms and lung function testing. Management includes bronchodilators, anti-inflammatories, and education to avoid triggers and use inhalers properly.