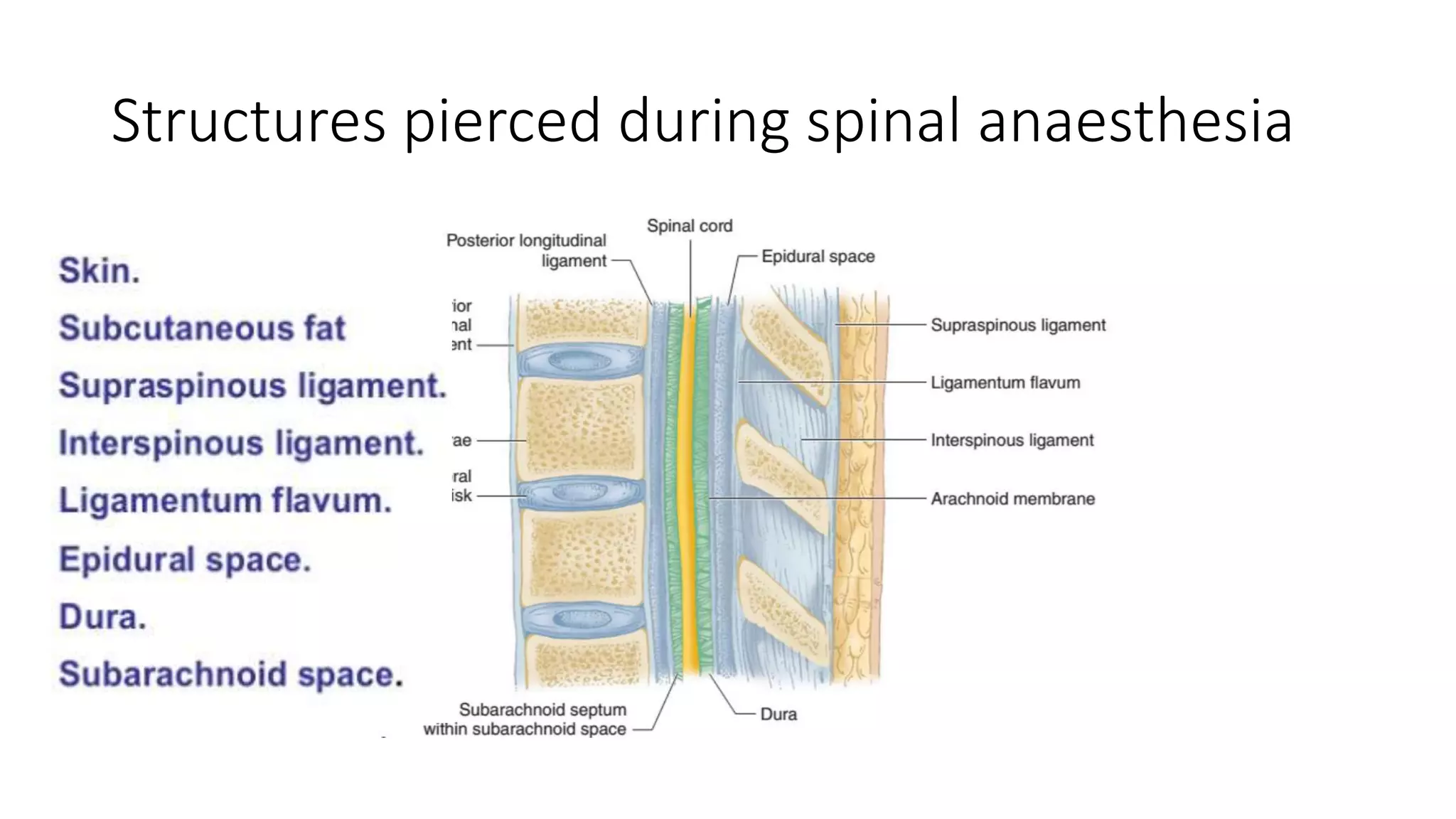
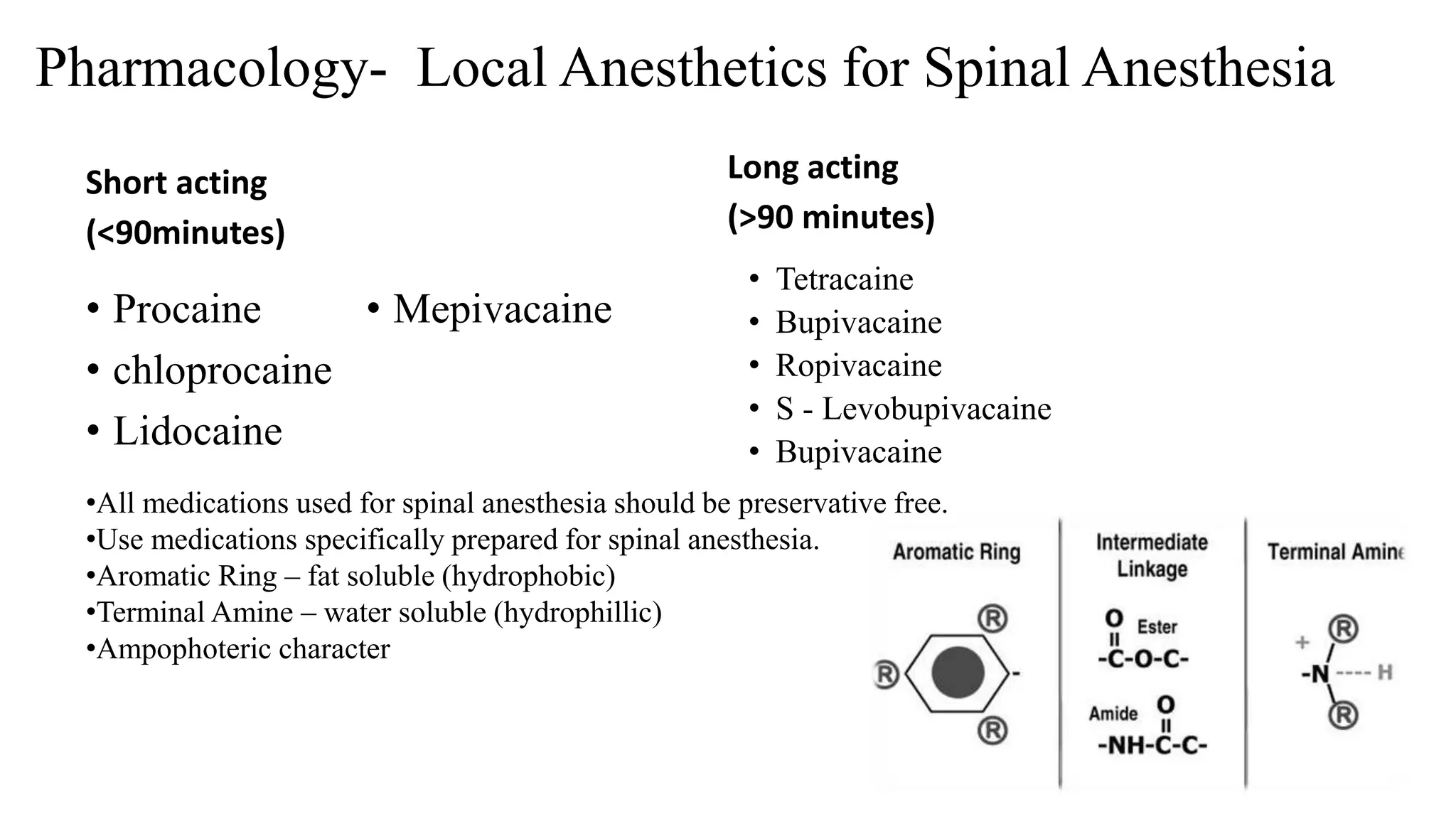
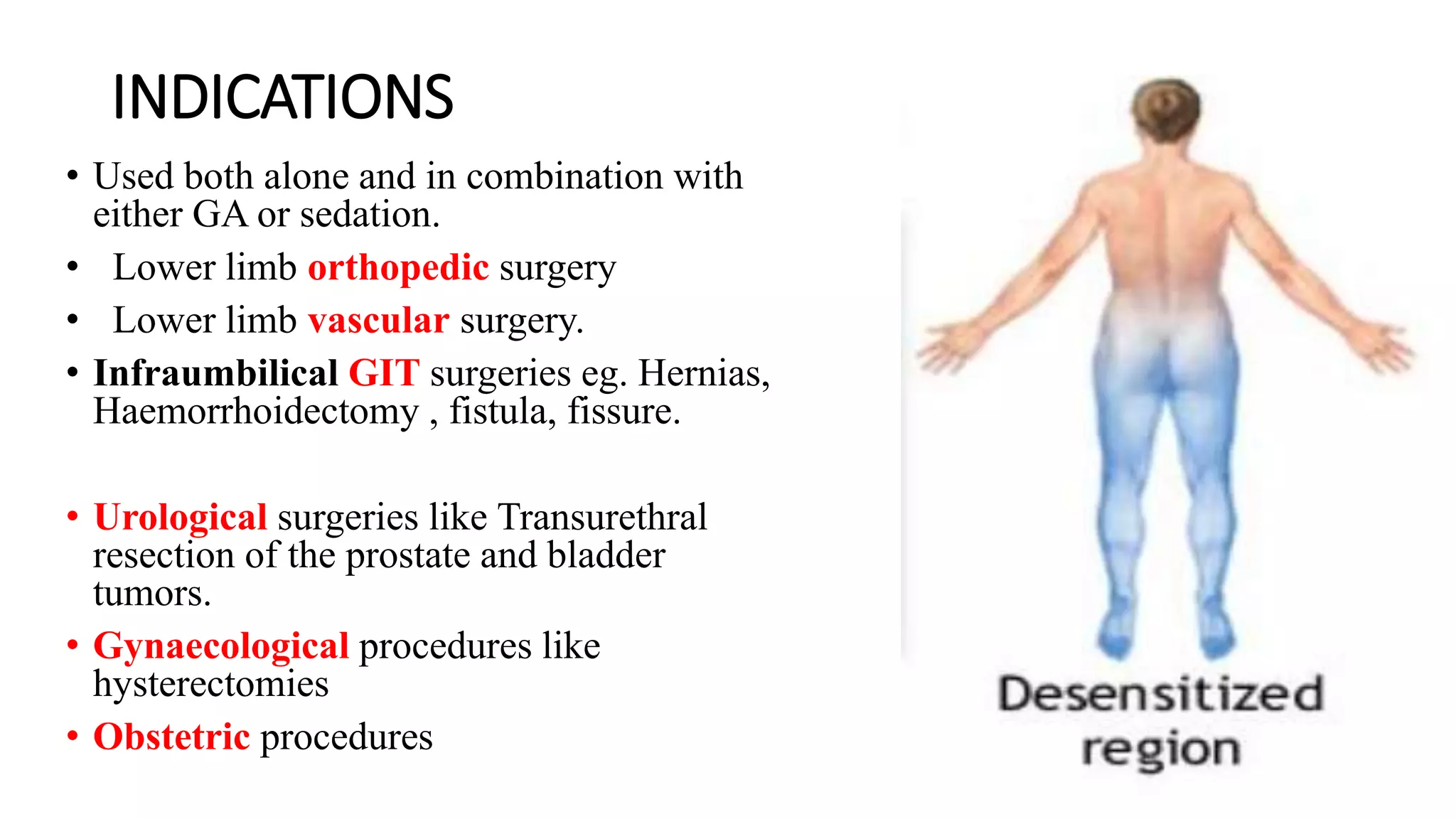
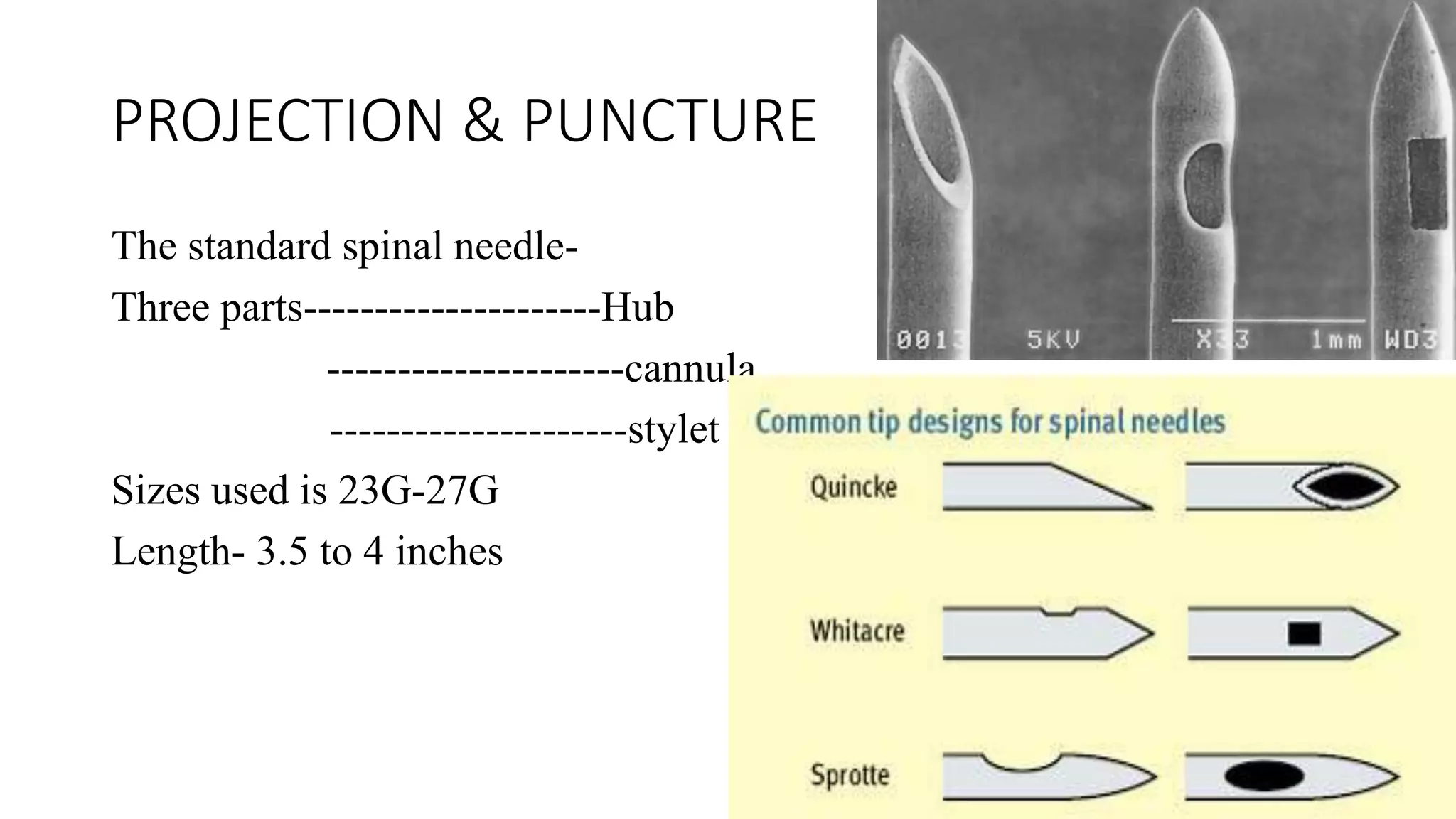
This document provides an overview of spinal anaesthesia. It begins with definitions and history, then covers anatomy including the subarachnoid space and structures pierced during spinal anaesthesia. It describes the mechanism of action of spinal anaesthesia and how local anaesthetics work. Indications, contraindications, preparation, positioning, and complications are discussed. Pharmacology of local anaesthetics for spinal anaesthesia and additives are outlined. Monitoring during the procedure and factors affecting the spread of local anaesthetics are also summarized.