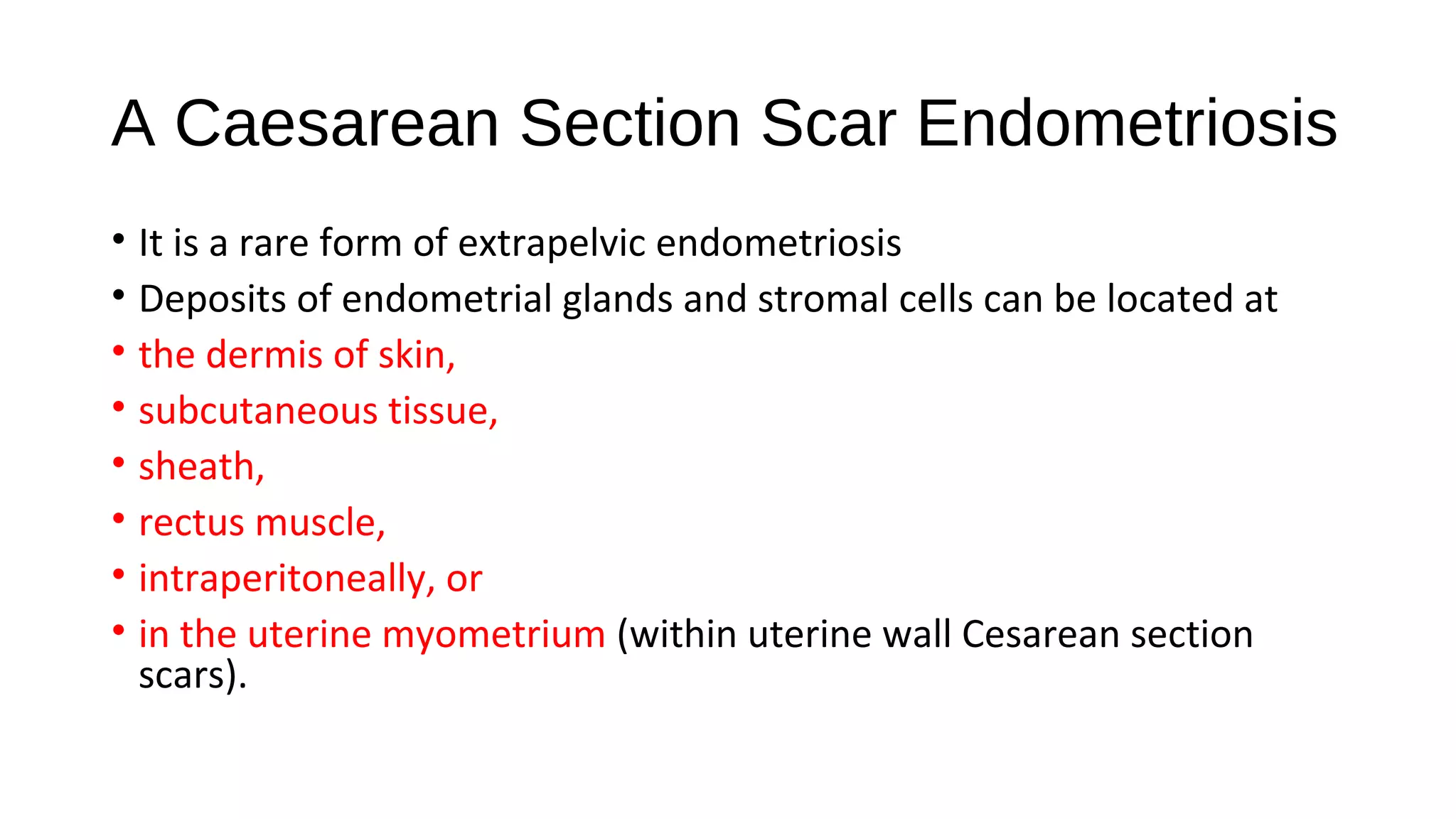
Cutaneous cesarean scar endometriosis is a rare type of endometriosis where endometrial tissue grows outside the uterus in the cesarean section scar. It occurs when endometrial cells are transplanted into the scar during cesarean section surgery. Patients experience cyclical pain with their menstrual cycle. Treatment involves complete surgical excision of the tissue with clear margins to prevent recurrence. Thorough cleaning of surgical sites during cesarean sections may help reduce the risk of developing this condition.