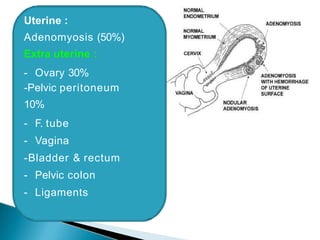
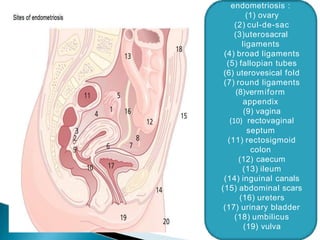
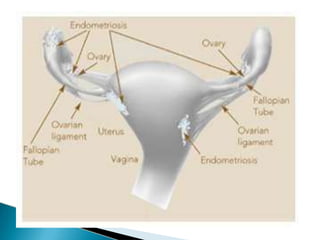
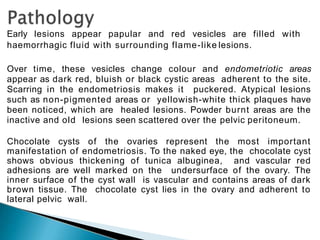
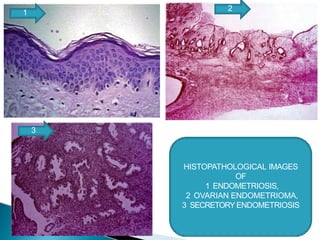
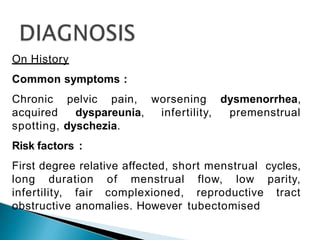
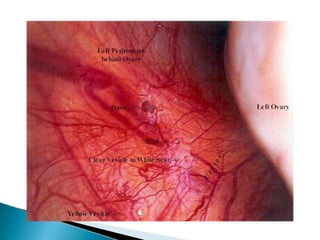
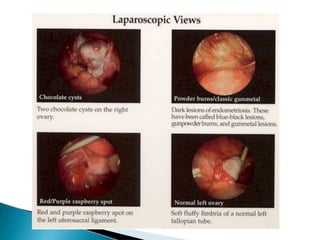
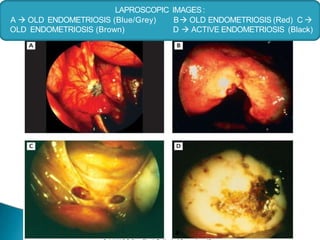
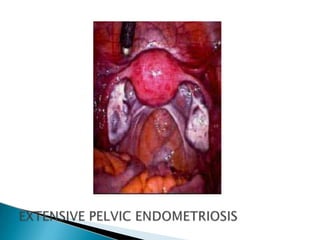
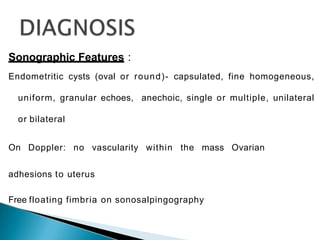
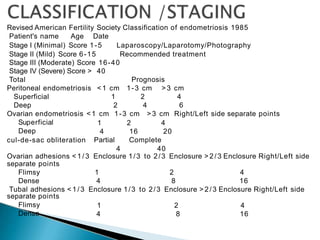
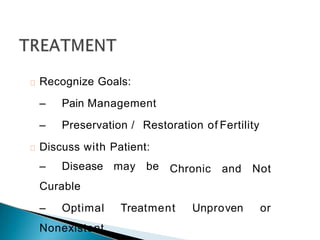
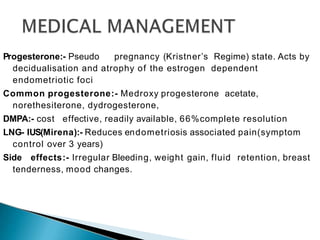
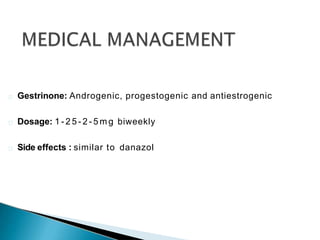
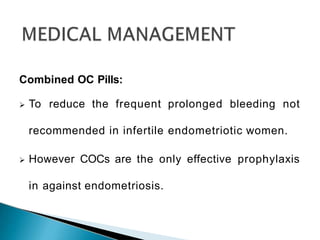
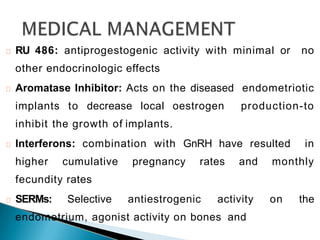
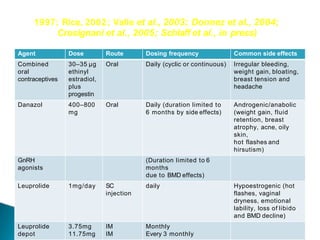
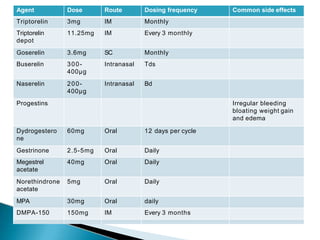
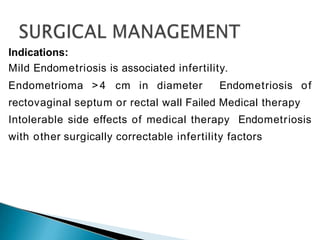
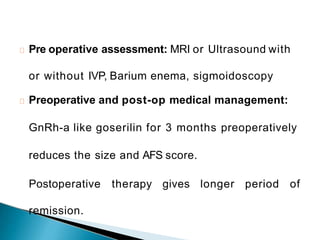
Endometriosis is the presence of endometrial tissue outside the uterus that induces a chronic inflammatory reaction. There are several proposed theories for its pathogenesis, including retrograde menstruation, coelomic metaplasia, and metastasis. Symptoms include pelvic pain and infertility. Diagnosis is typically made by laparoscopy to visualize lesions. Treatment involves pain management, preservation of fertility, and involves medical therapy with hormones or NSAIDs and surgery. The goal of management is individualized based on the patient's symptoms, disease severity, and fertility desires.