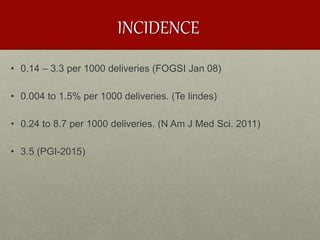
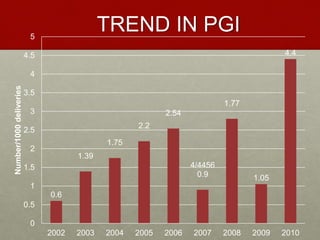
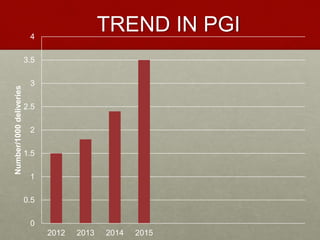
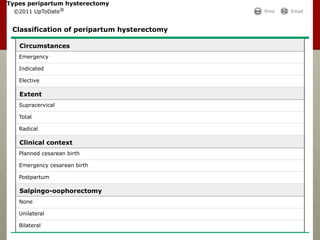
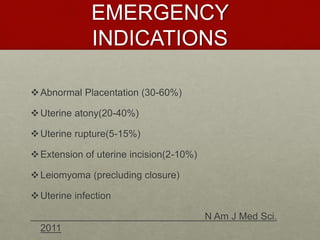
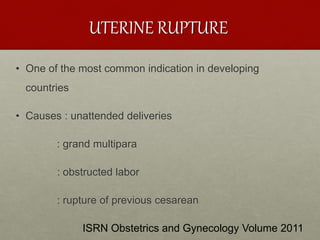
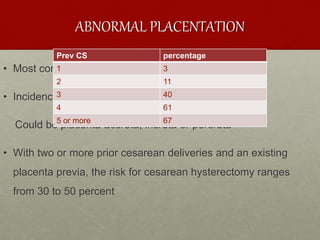
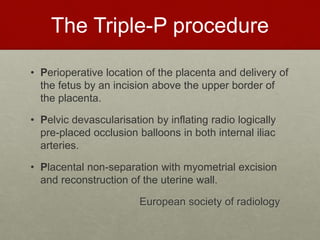
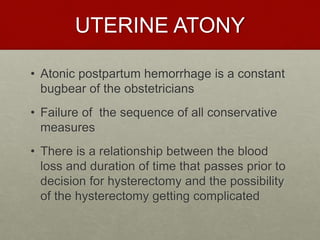
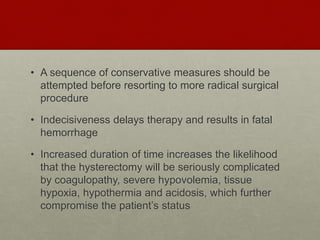
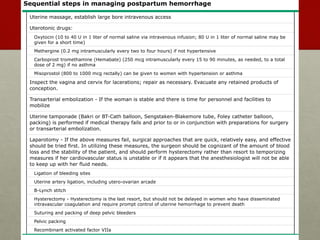
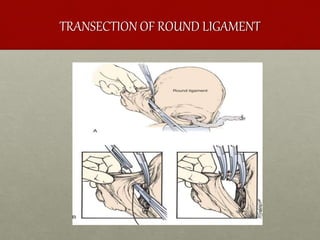
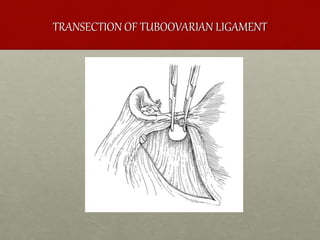
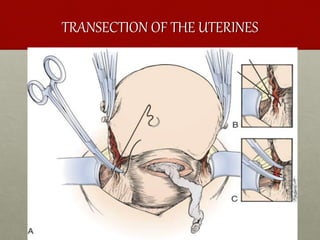
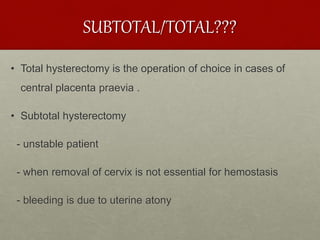
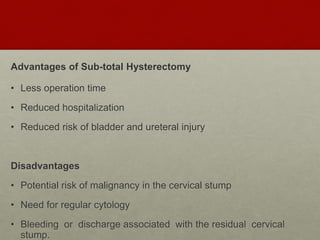
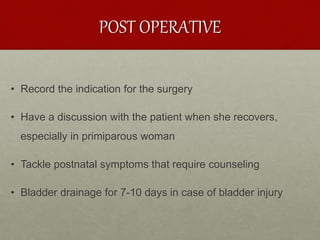
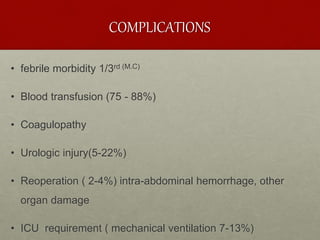
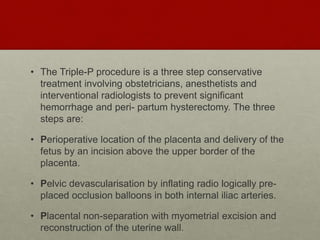
The document discusses peripartum hysterectomy, including its definition, history, incidence and trends, risk factors, types, indications, complications, and techniques. A key point is that a sequence of conservative measures should be attempted before hysterectomy to control uterine hemorrhage, as indecisiveness can lead to fatal excessive bleeding. The "Triple-P procedure" is also summarized as a three-step conservative approach involving obstetric, anesthesia and interventional radiology teams to prevent hemorrhage and need for hysterectomy in high-risk cases.