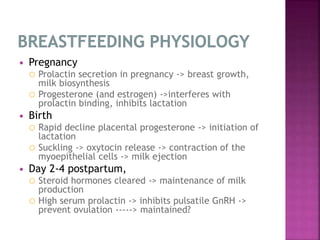
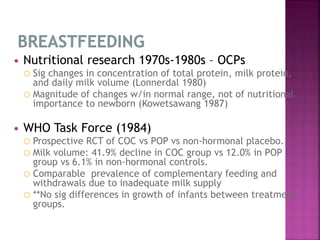
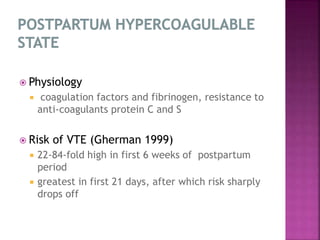
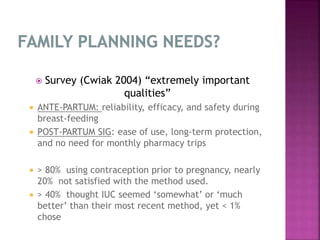
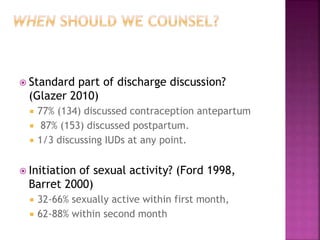
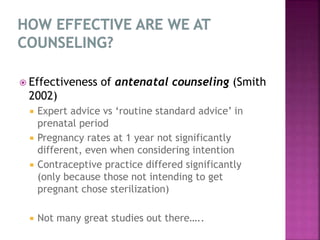
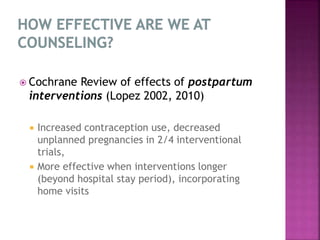
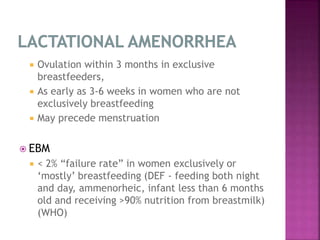
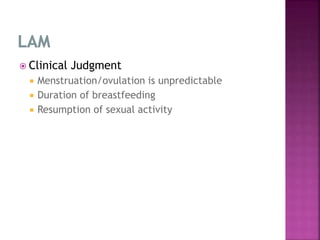
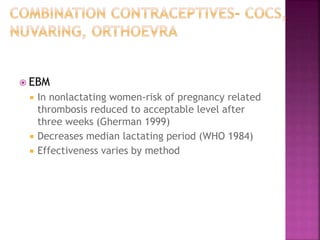
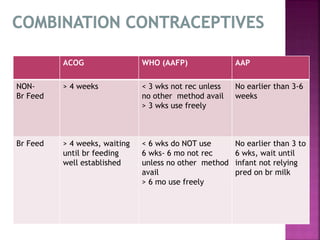
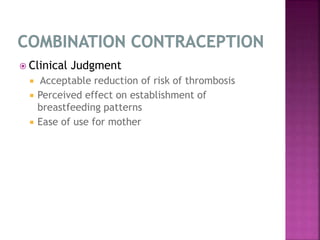
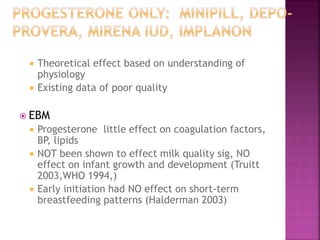
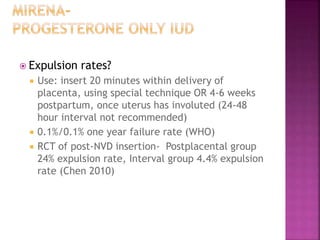
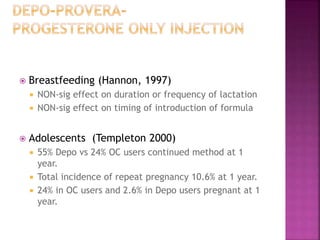
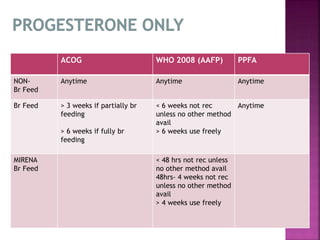
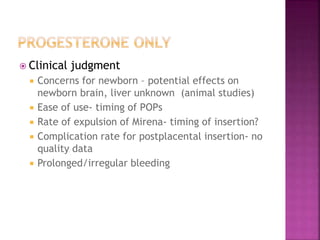
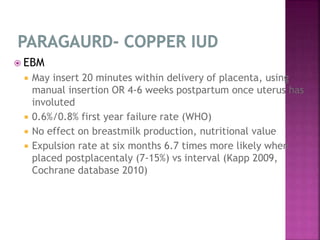
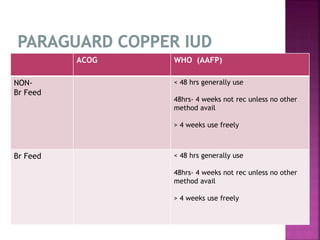
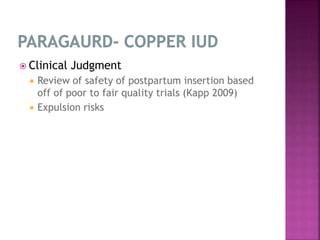
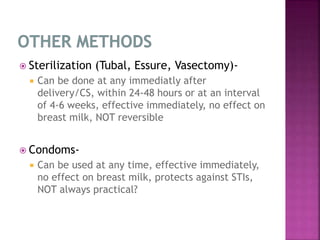
Contraception in the postpartum period differs due to breastfeeding, increased risk of blood clots, and unpredictable ovulation. Counseling should occur during antenatal and postnatal periods. Options include breastfeeding, progestin-only pills, implants, IUDs, sterilization, condoms. Timing of use depends on breastfeeding status and bleeding risk. Recommendations balance effectiveness, safety, and ease of use while supporting breastfeeding.