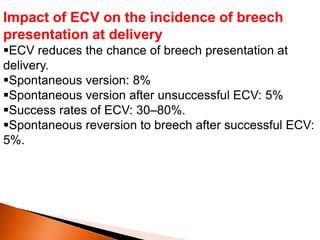
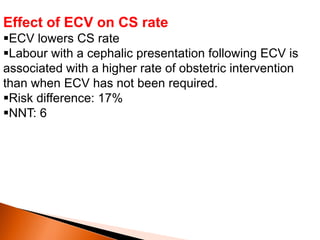
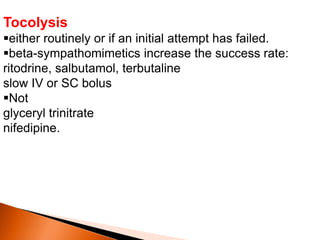
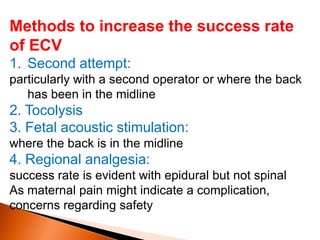
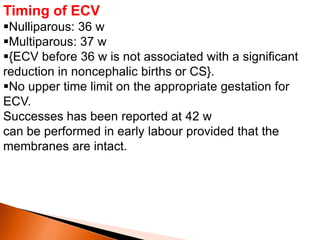
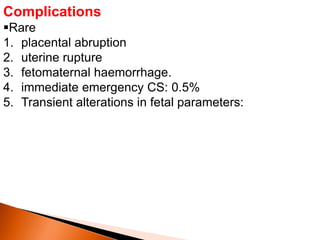
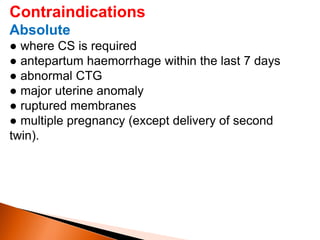
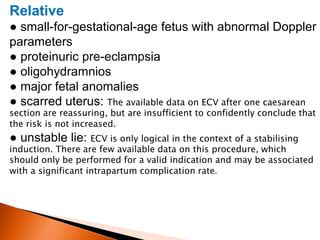
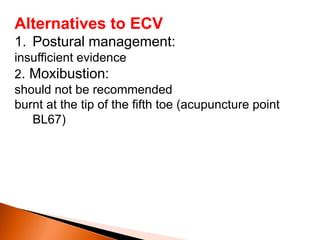
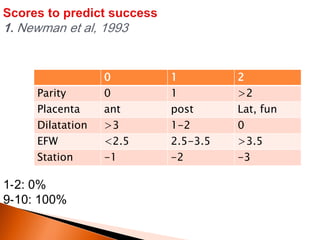
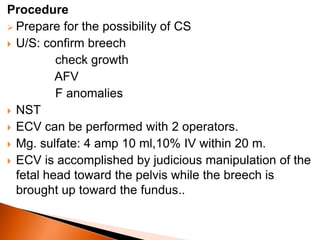
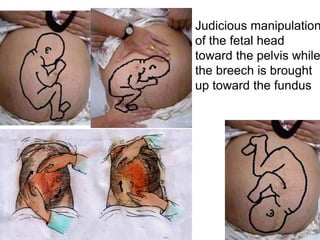
This document discusses external cephalic version (ECV), a procedure used to manually turn a breech baby into a head-down position before birth. It notes that ECV reduces the need for cesarean section and that success rates range from 30-80%. Factors that increase the likelihood of success include multiparity, uterine relaxation, an unengaged breech, and a palpable fetal head. Complications are rare but can include placental abruption or emergency cesarean. ECV is generally safe when performed after 36 weeks of gestation.