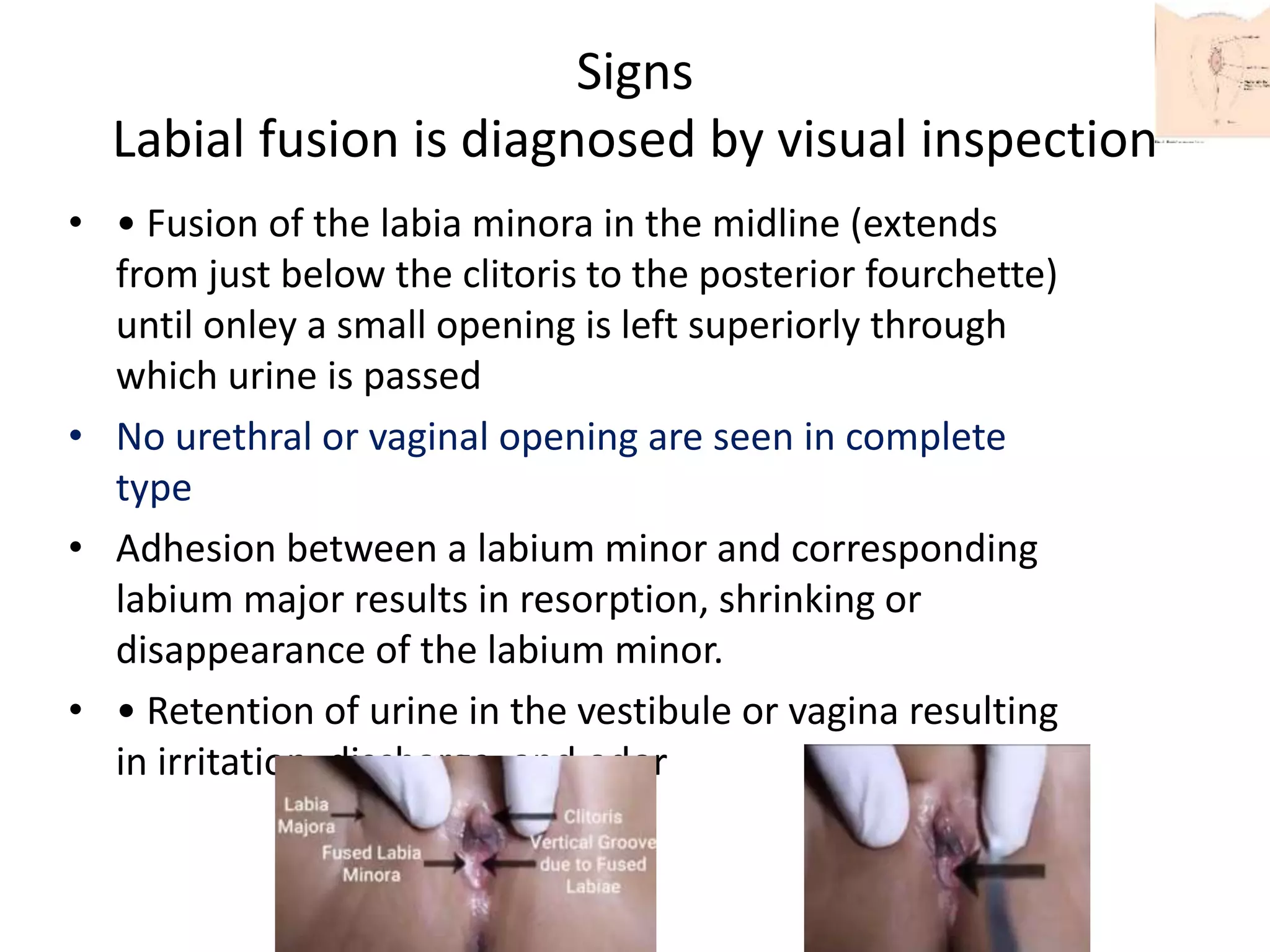
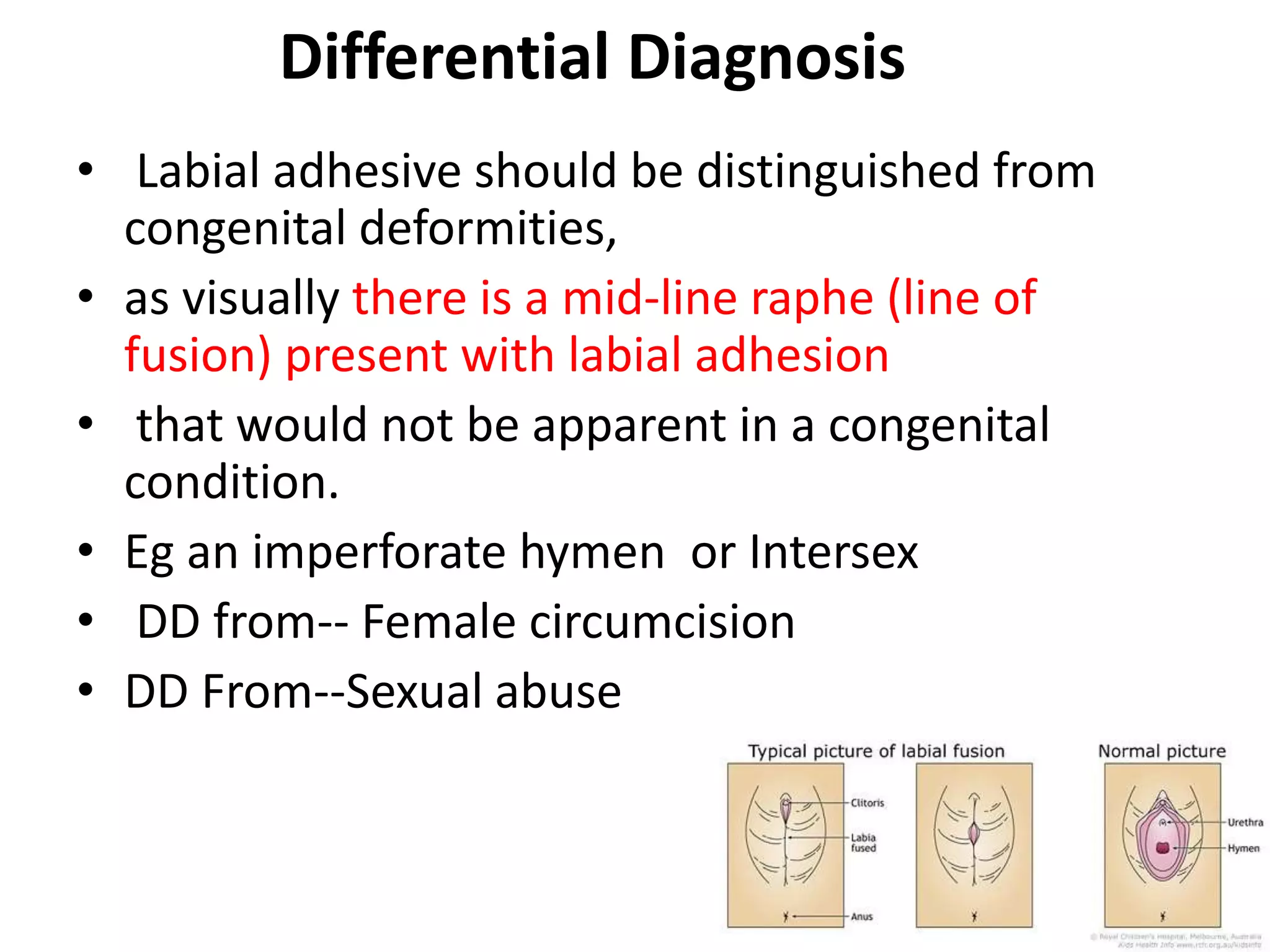
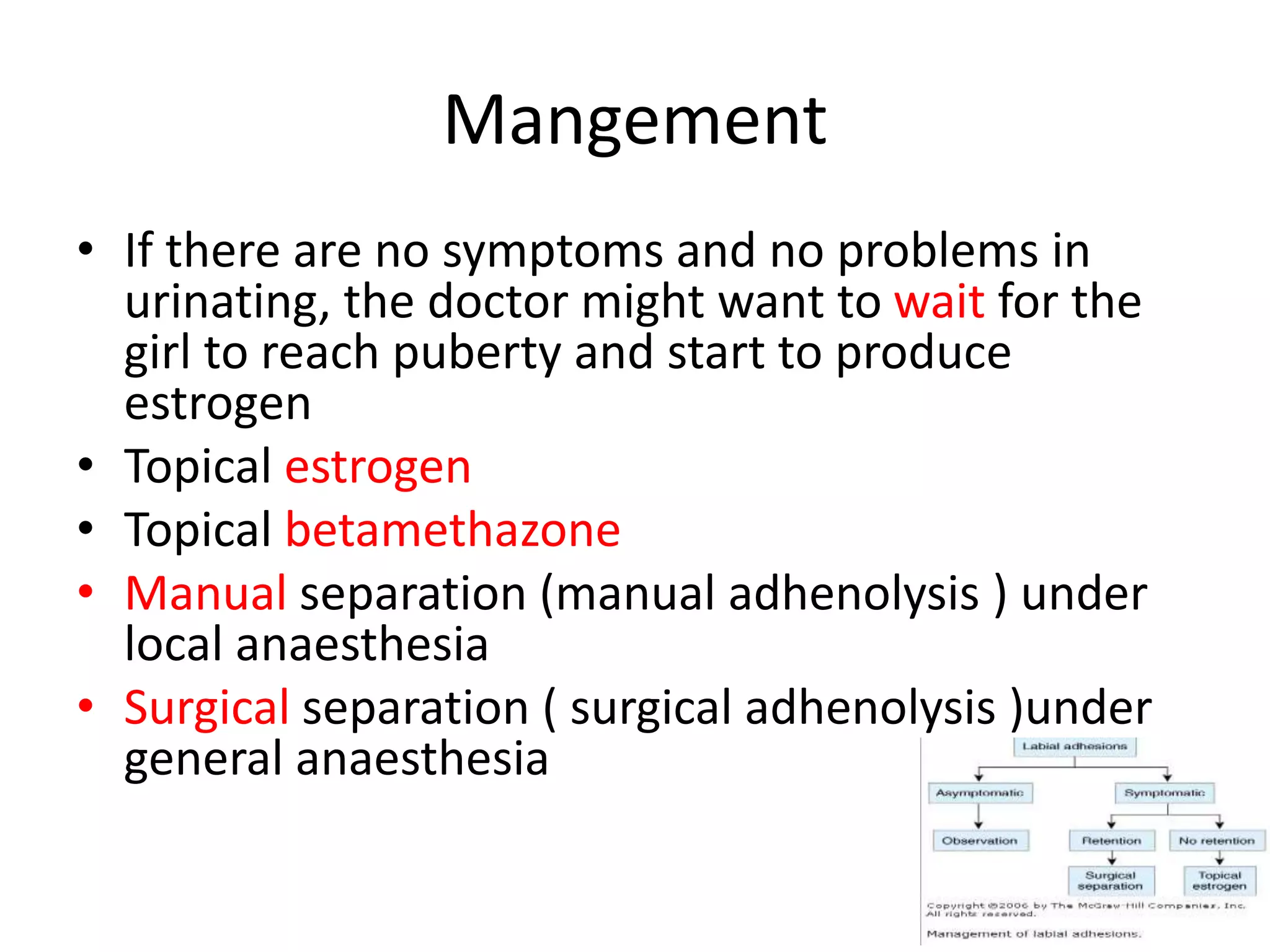
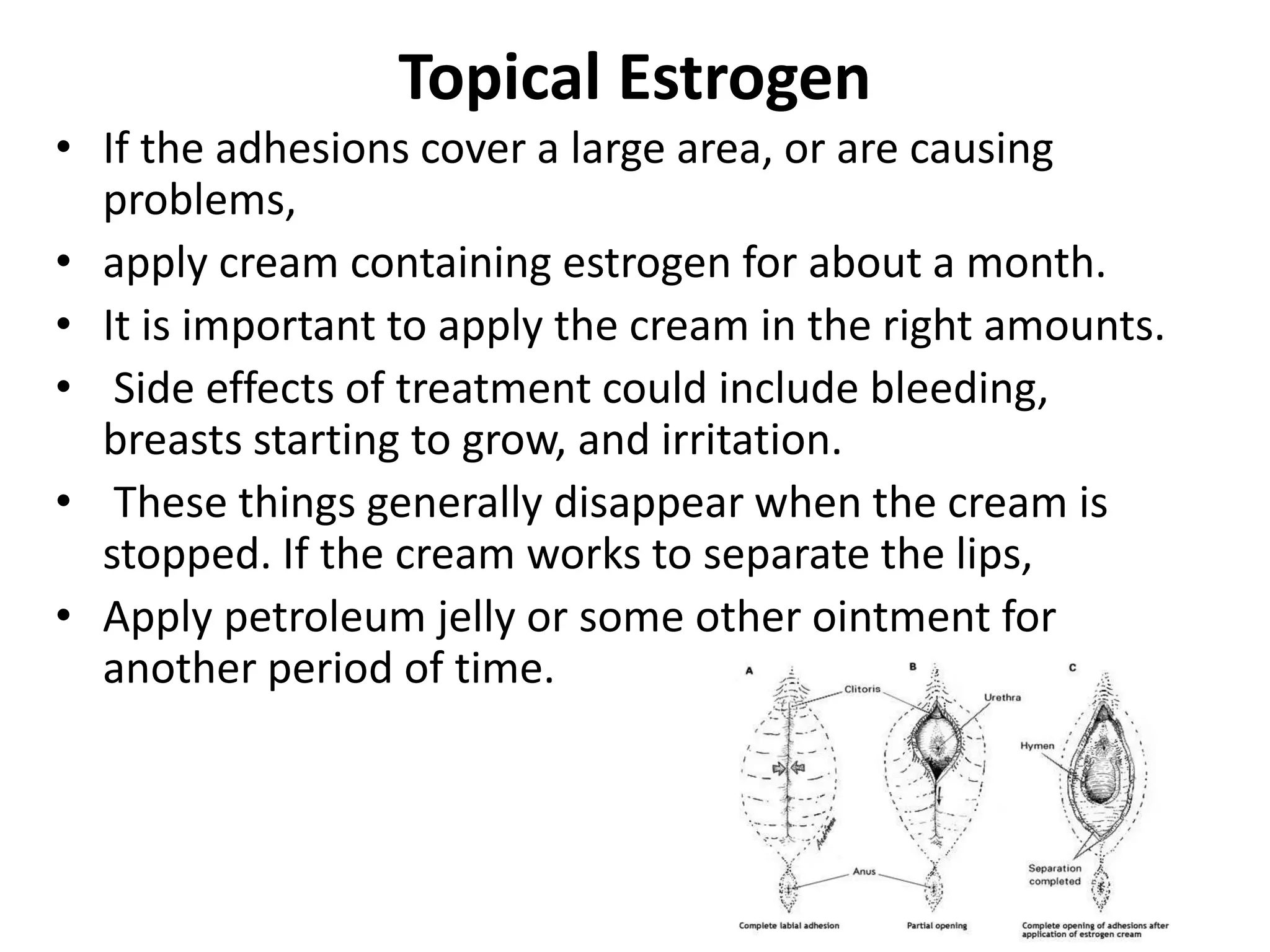
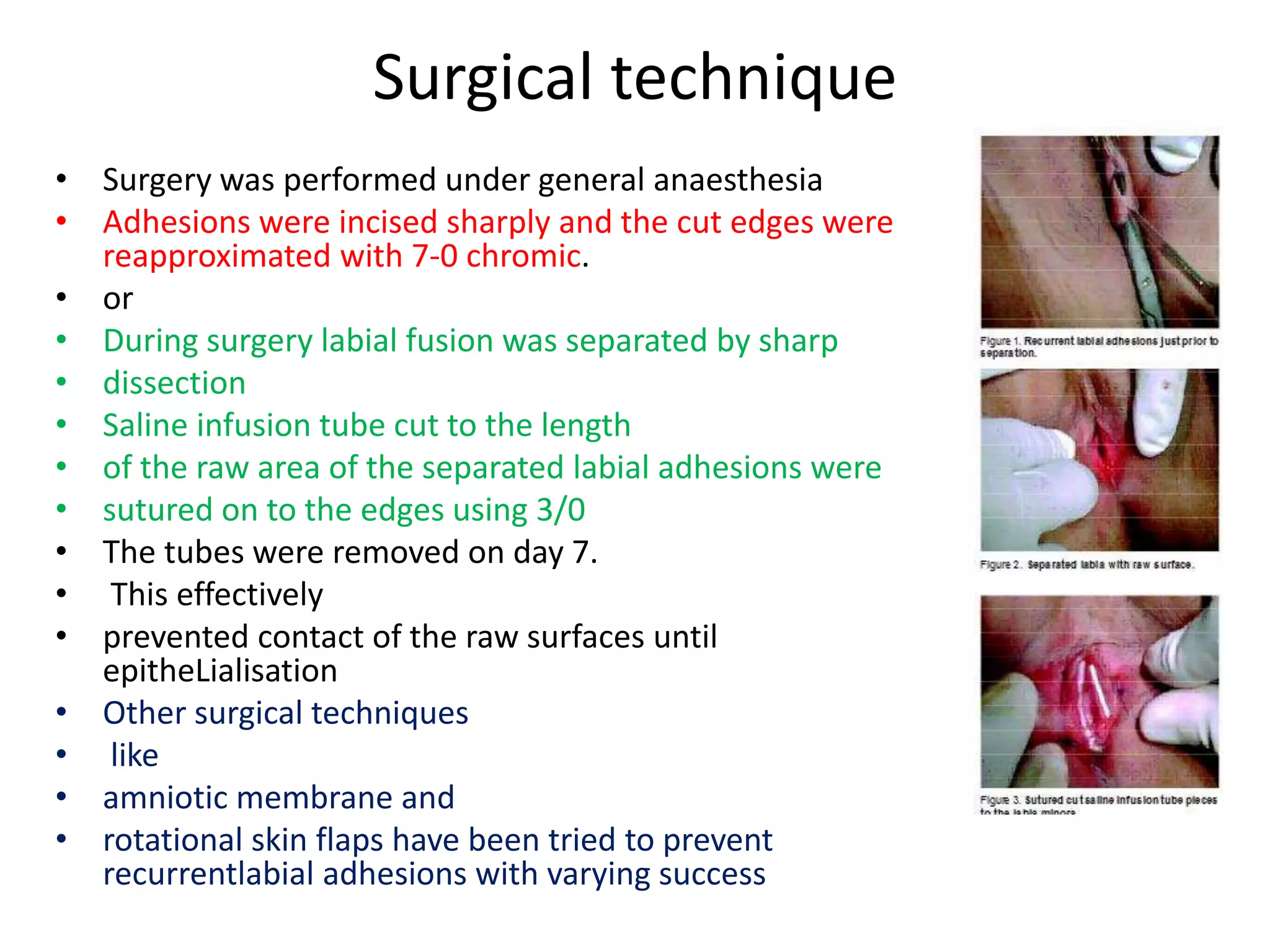
Labia minora adhesions (LMA) are the partial or complete fusion of the labia minora. They occur in 0.6-3.3% of prepubertal girls and are usually asymptomatic, resolving spontaneously during adolescence. Potential causes include microtraumas from overcleaning or chronic irritation/inflammation. Treatment is usually not needed unless causing symptoms like urinary issues. Options include topical estrogen or steroid creams, or manual separation under local anesthesia. Surgery is rarely required and recurrence can be prevented with gentle separation and avoiding irritants.