This document discusses various techniques used in blood banking and transfusion medicine, including:
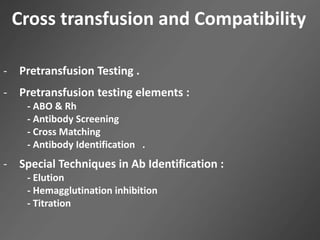
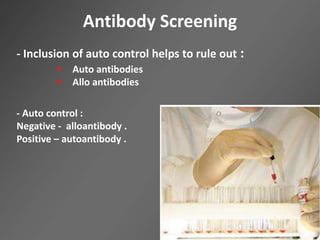
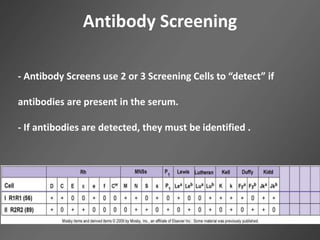
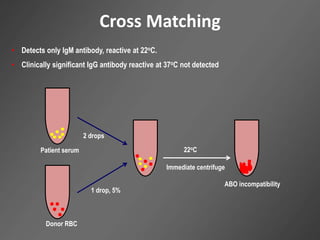
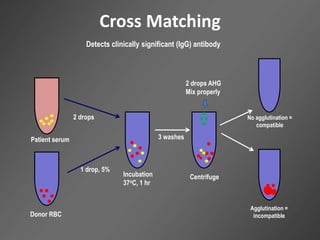
1. Pretransfusion testing involves ABO/Rh typing, antibody screening, and crossmatching to select compatible blood and prevent hemolytic transfusion reactions.
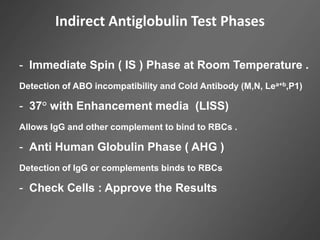
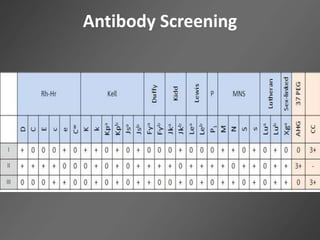
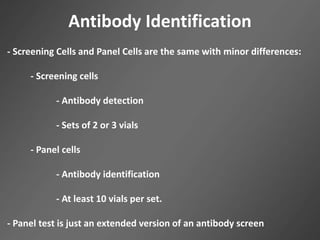
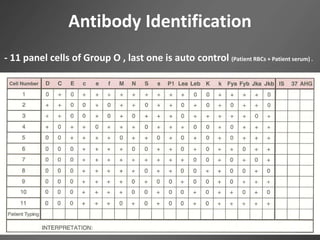
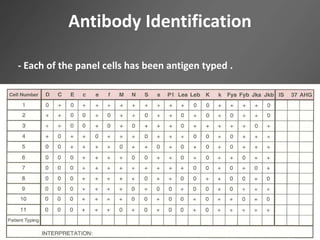
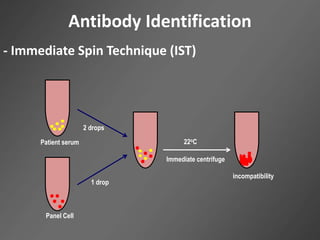
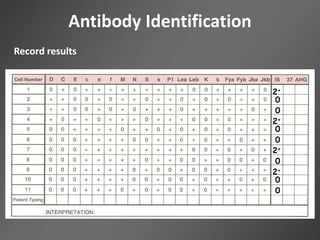
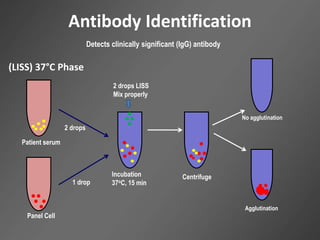
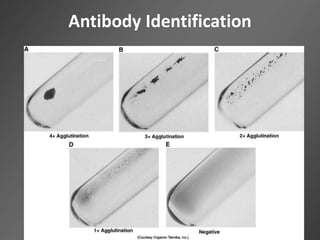
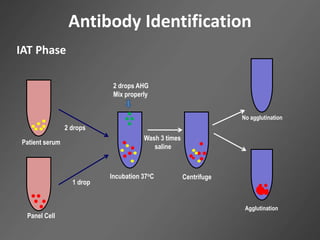
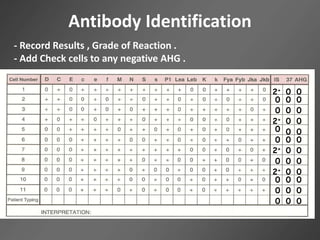
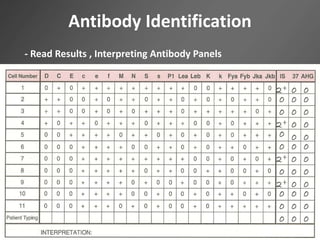
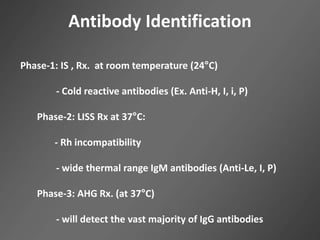
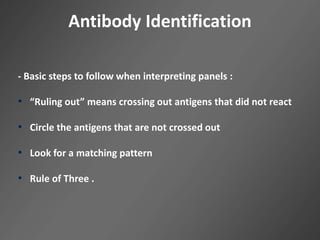
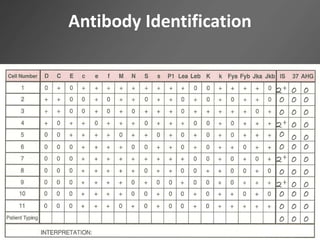
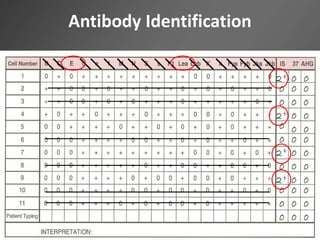
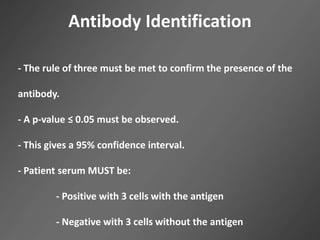
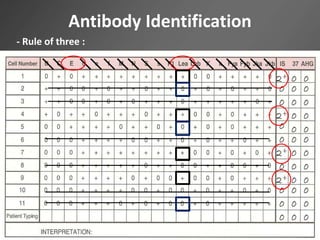
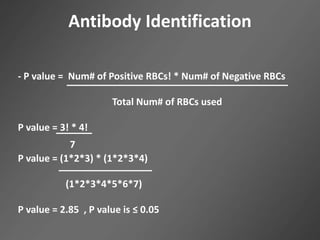
2. Antibody identification uses a panel of red blood cells to identify the specific antibody in a patient's serum through various testing phases including immediate spin, LISS incubation, and antiglobulin.
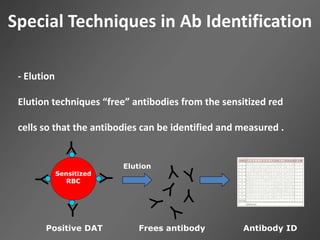
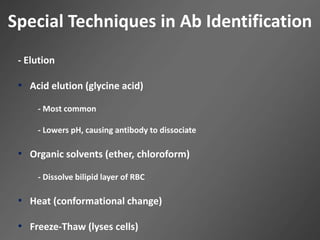
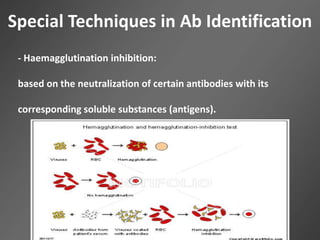
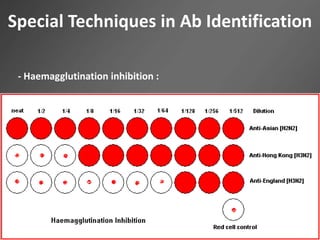
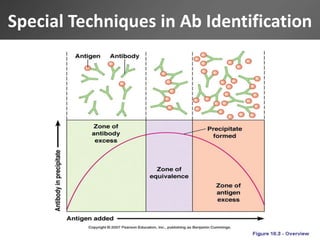
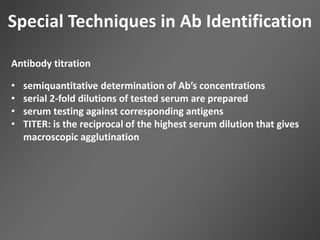
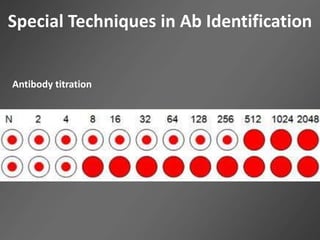
3. Special techniques like elution, hemagglutination inhibition, and titration are used to further characterize antibodies or quantify their concentration.