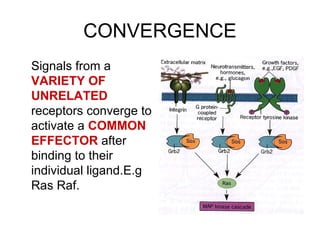
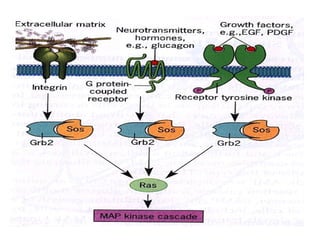
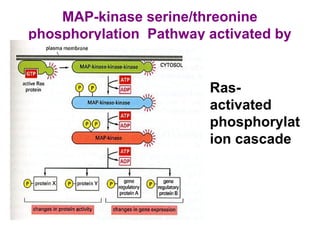
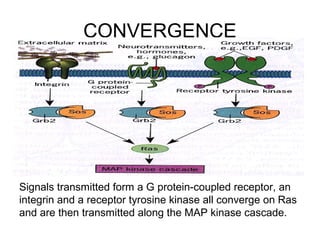
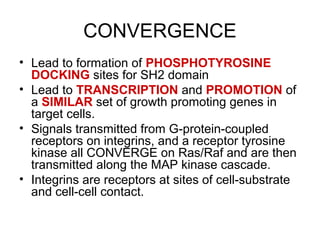
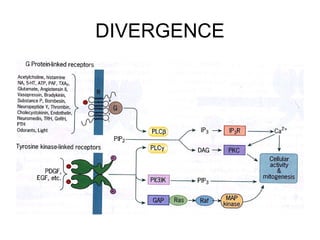
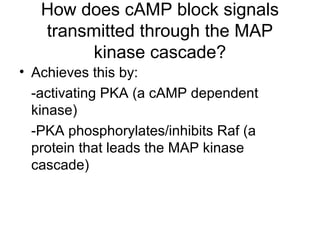
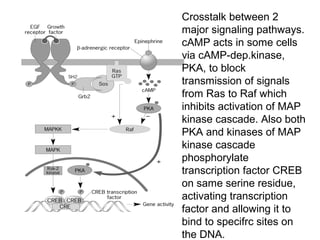
Signals from unrelated receptors can converge on common effectors like Ras/Raf, while signals from the same ligand can diverge and activate different effectors. Signals can also be passed between pathways through crosstalk. Cell signaling pathways integrate information from different sources to mount an appropriate cellular response.