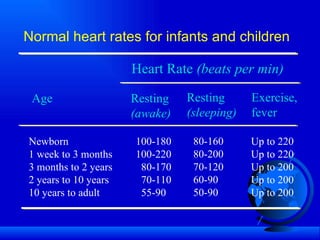
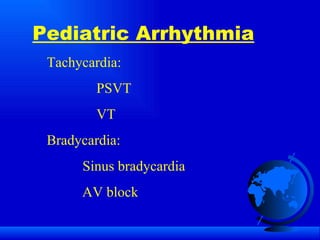
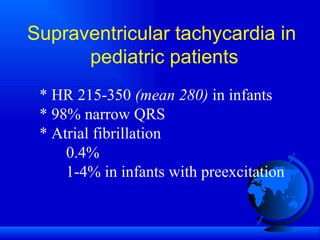
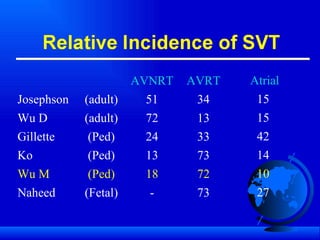
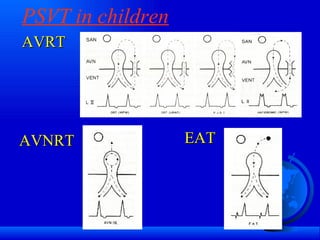
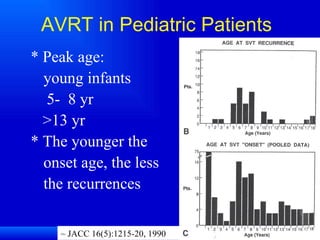
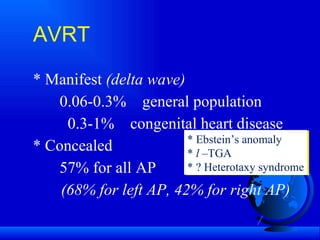
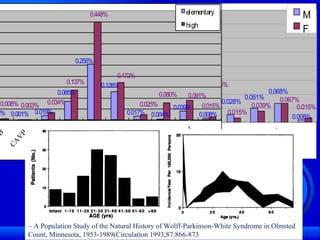
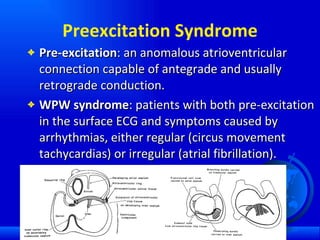
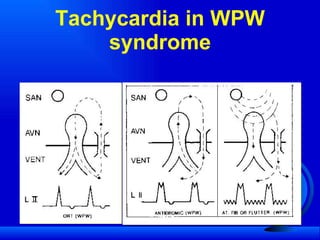
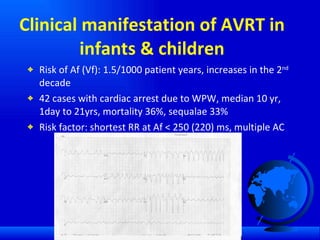
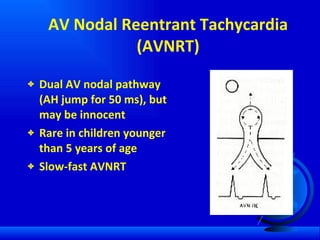
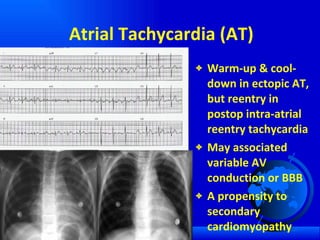
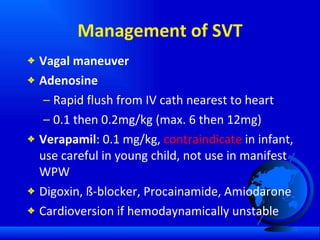
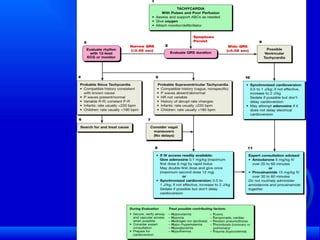
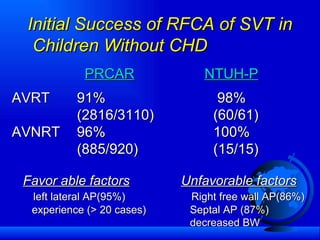
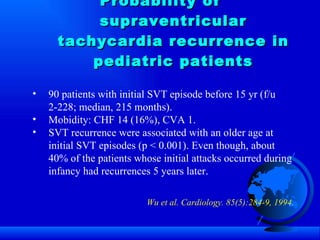
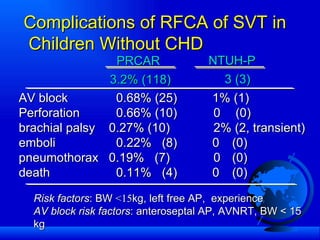
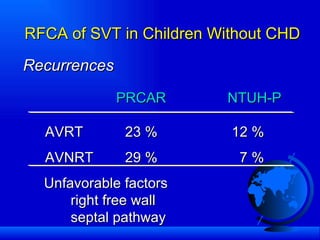
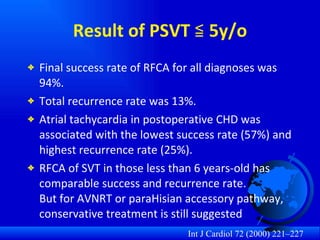
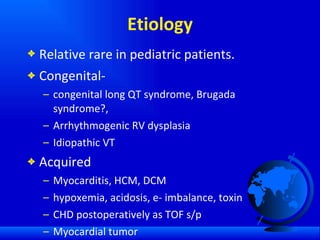
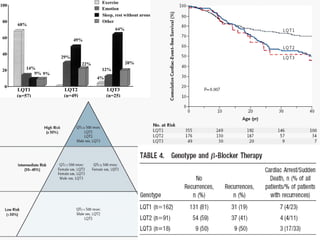
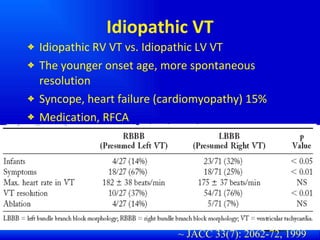
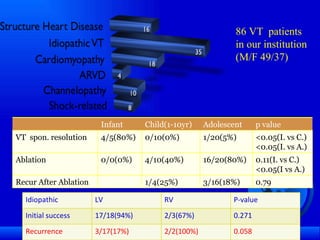
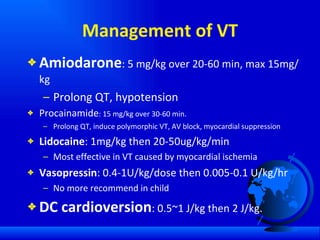
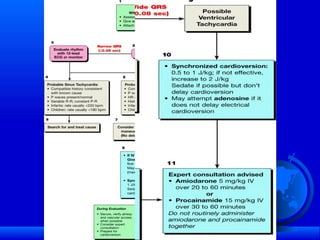
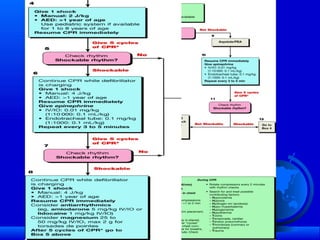
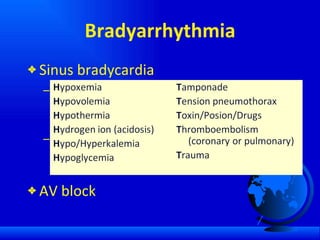
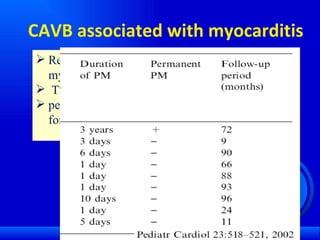
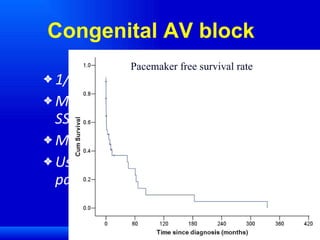
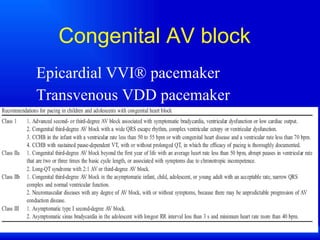
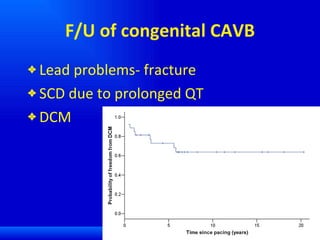
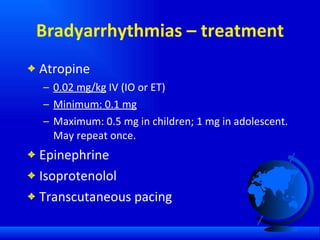
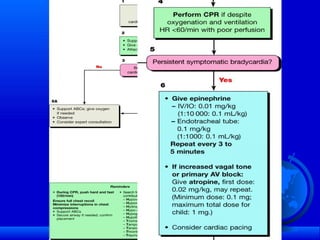
The document discusses various pediatric arrhythmias including tachycardias and bradycardias. It provides details on normal heart rates at different ages and describes common supraventricular tachycardias like AV nodal reentrant tachycardia, accessory pathway mediated tachycardias. It also discusses idiopathic ventricular tachycardia and management strategies for different arrhythmias including medication and ablation. Congenital complete heart block is described along with its association with maternal autoimmune conditions.