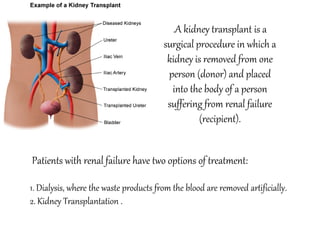
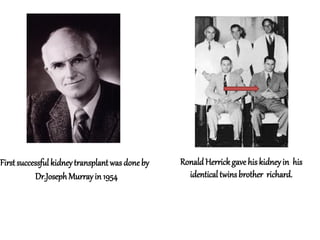
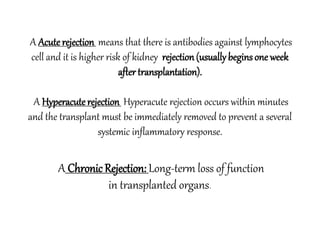
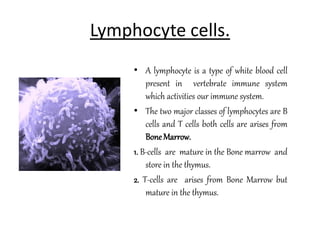
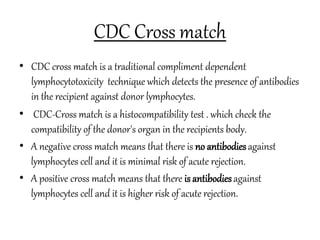
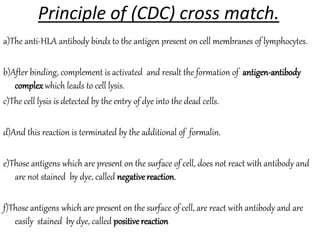
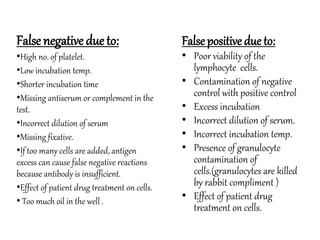
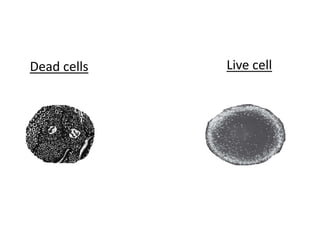
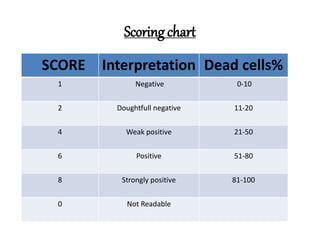
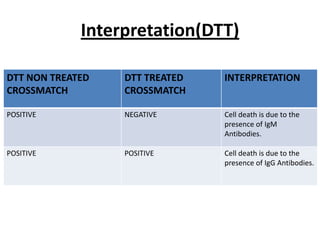
The document provides information about kidney transplantation and the CDC crossmatch test. It discusses the two main treatment options for renal failure - dialysis and kidney transplantation. It then describes the CDC crossmatch test, which checks for antibodies in the recipient that could reject the donor kidney by detecting if antibodies bind to lymphocytes. A negative crossmatch means there is low risk of acute rejection, while a positive crossmatch indicates a higher risk.