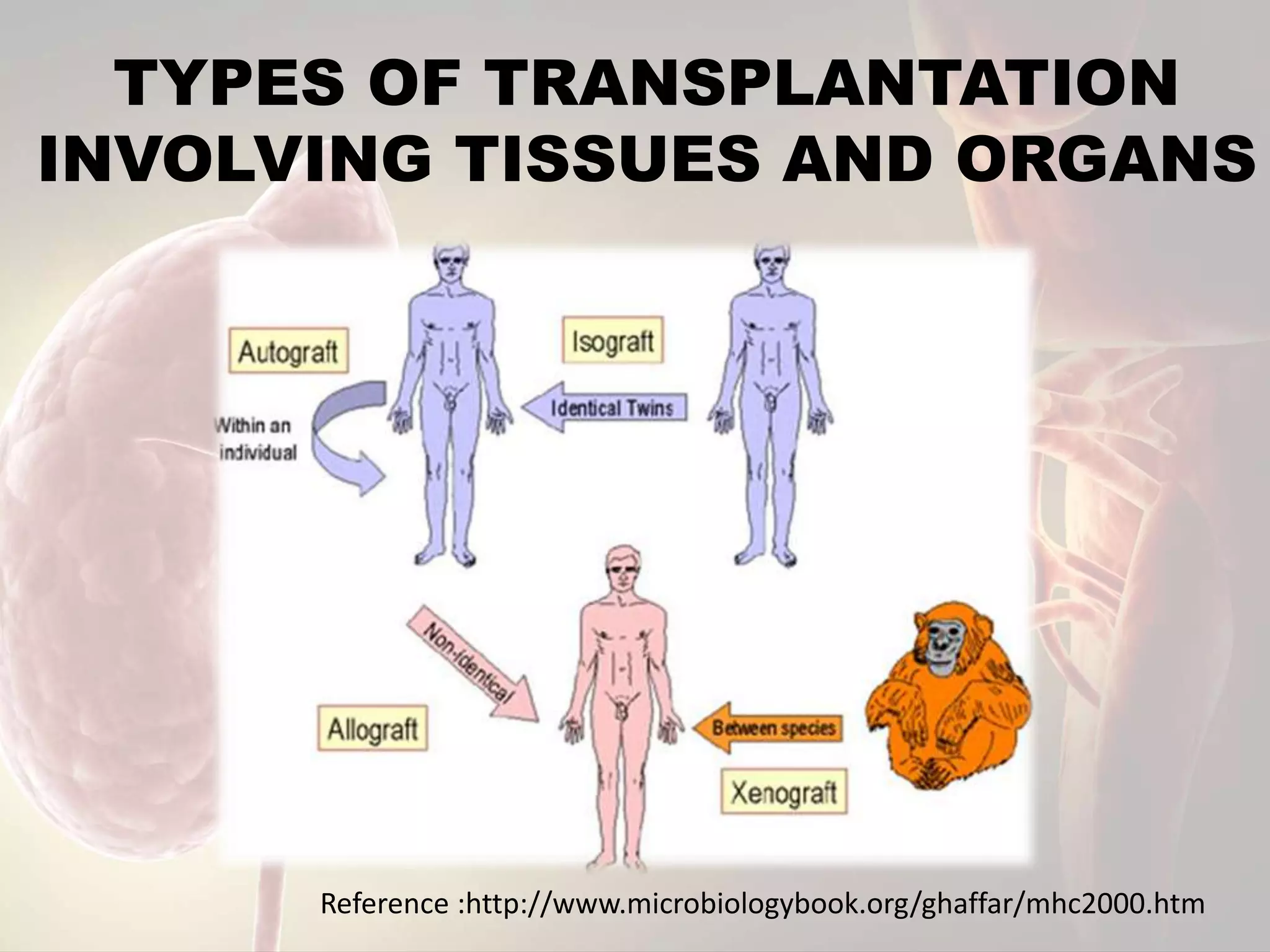
The document discusses transplantation and the immune response. It begins by defining transplantation as moving cells, tissues, or organs from one site to another, either within an individual or between donors and recipients. There are several types of transplantation - autografts within an individual, isografts between identical twins, allografts between non-identical individuals of the same species, and xenografts between different species. Rejection can be acute, occurring within 6 months, or chronic with repeated acute episodes ultimately causing transplant failure. Immunosuppressive drugs are used to reduce rejection by dampening the immune response.