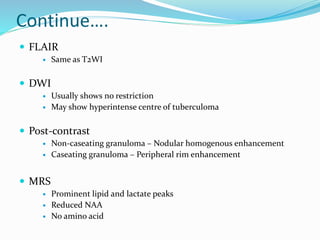
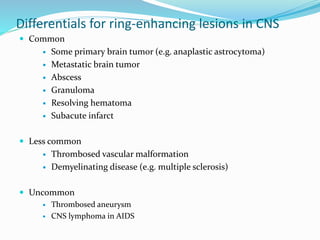
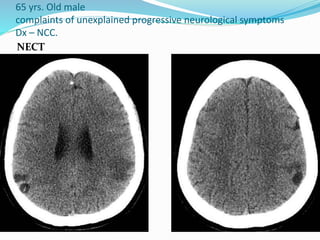
This document discusses Mycobacterium tuberculosis and central nervous system tuberculosis, focusing on intracranial tuberculomas. It describes the etiology, clinical features, imaging appearance and characteristics of tuberculomas on CT and MRI. Tuberculomas appear as ring-enhancing lesions on imaging and can be distinguished from other ring-enhancing lesions like abscesses, metastases and neurocysticercosis based on their imaging characteristics and presence of a caseous necrotic core. Differential diagnosis and pathology of tuberculomas are also discussed.