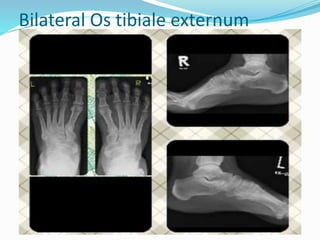
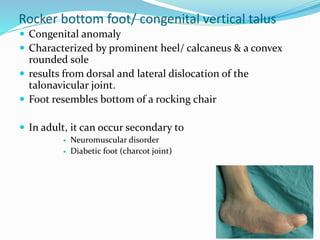
This document provides an overview of various conditions involving the foot and ankle that can be evaluated on radiology imaging. It discusses accessory ossicles that can occur in the foot and be a cause of pain. It also reviews conditions like rocker bottom foot, tarsal coalition, fractures around the ankle joint involving the lateral malleolus, tibial plafond, talus and calcaneus. Other topics covered include osteochondral defects of the talus, accessory ossicles of the foot, and angles used to evaluate calcaneal fractures.