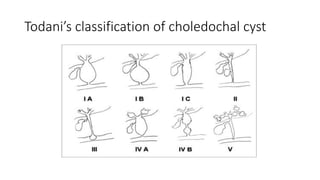
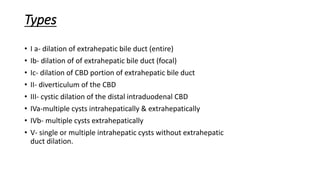
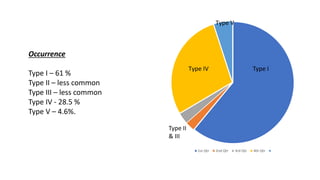
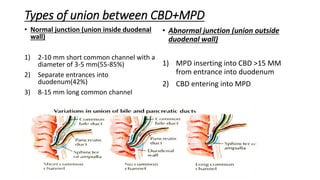
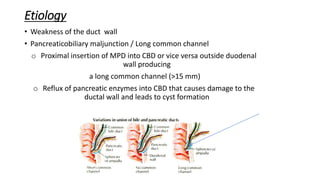
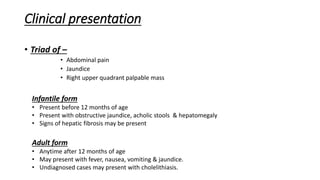
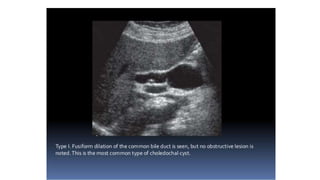
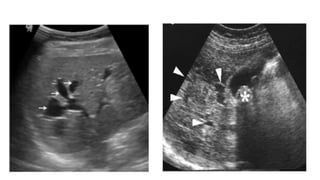
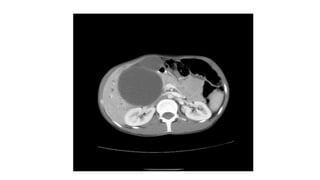
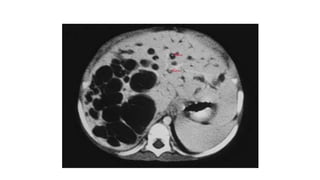
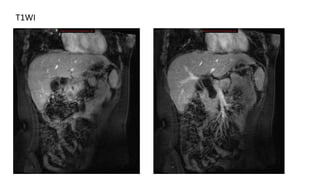
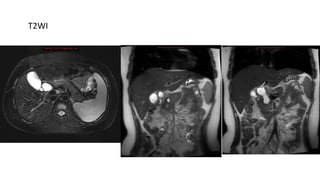
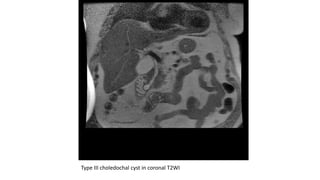
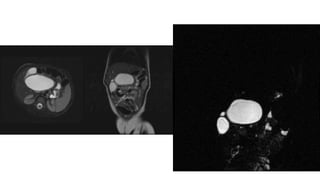
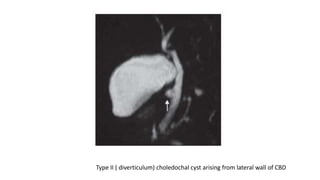
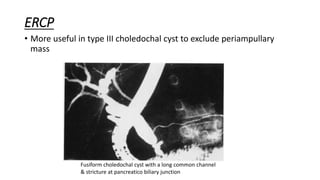
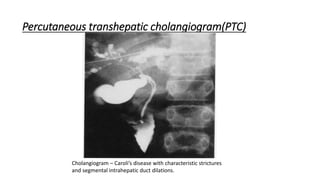
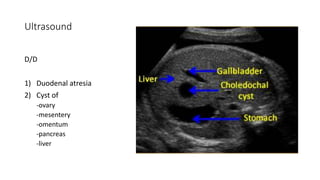
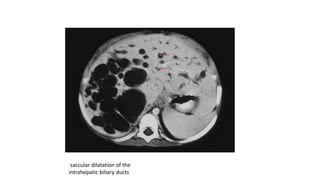
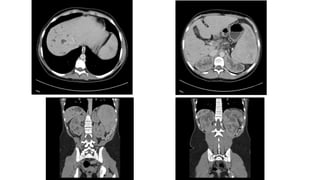
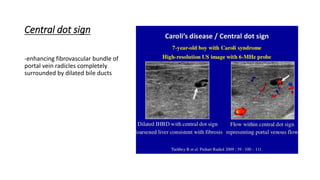
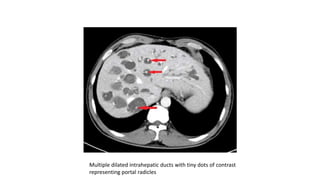
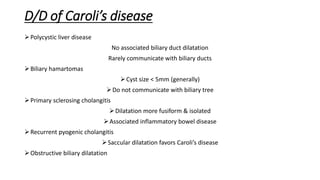
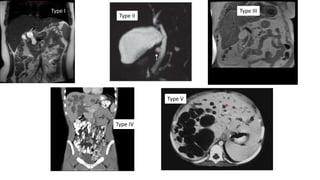
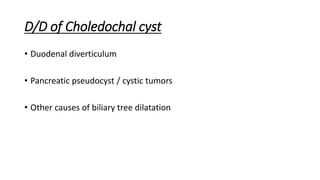
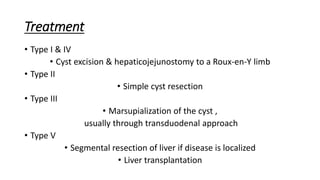
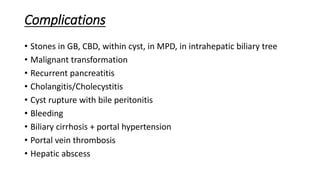
Choledochal cyst is a congenital anomaly involving cystic dilation of the bile ducts. It is classified into 5 types based on the location and extent of dilation. Type I is the most common. Imaging plays an important role in diagnosis and classification, with MRCP being the gold standard. Treatment involves complete excision of the cyst and Roux-en-Y hepaticojejunostomy. Complications include stones, malignancy, cholangitis and rupture. Caroli's disease is a rare disorder involving saccular dilation of intrahepatic bile ducts.