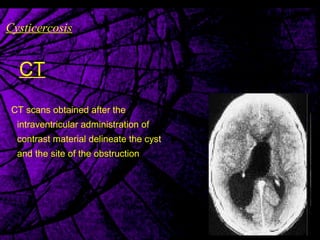
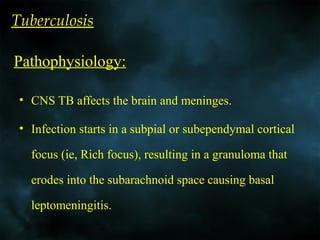
This document discusses various infections of the brain and meninges, including fungal infections, parasitic infections (toxoplasmosis and cysticercosis), and tuberculosis. It provides detailed information on the pathogenesis, imaging appearance on CT and MRI, and characteristics of lesions caused by these infectious agents. Key points include descriptions of the ring-enhancing lesions, edema, and enhancement patterns seen with toxoplasmosis and cysticercosis on imaging. It also outlines the leptomeningeal and basal cistern enhancement, ventriculomegaly, and infarcts associated with tuberculosis meningitis and parenchymal tuberculosis granulomas.