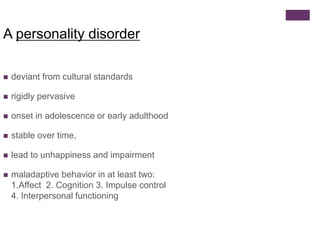
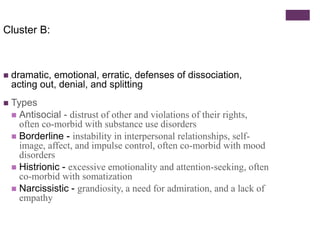
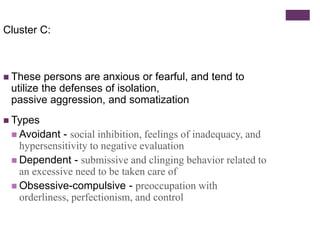
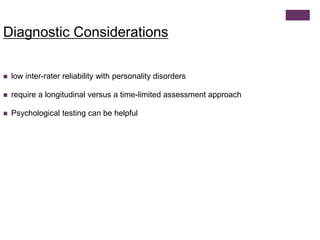
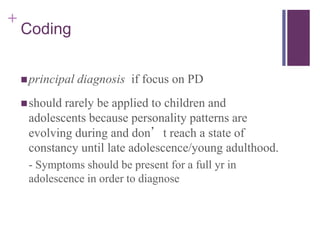
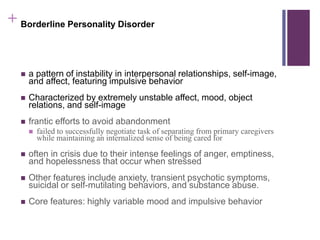
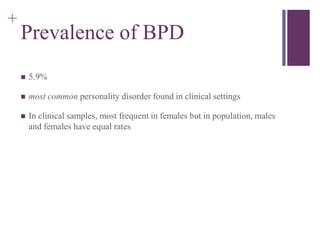
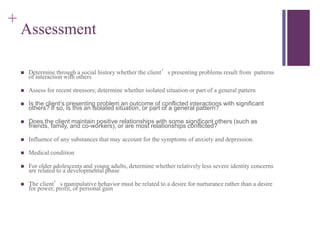
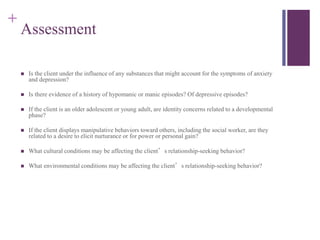
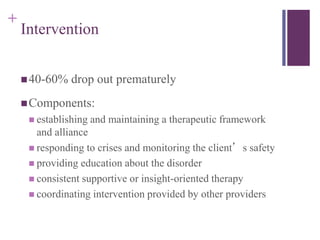
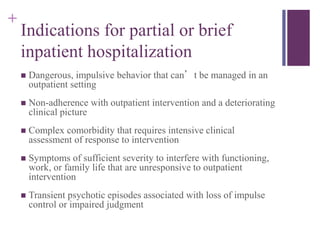
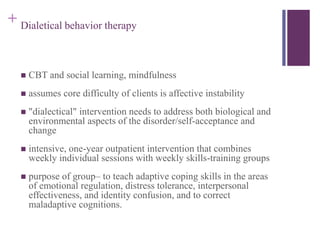
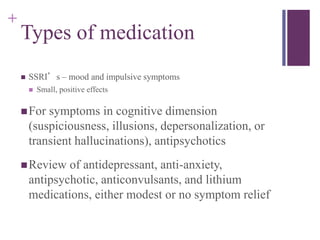
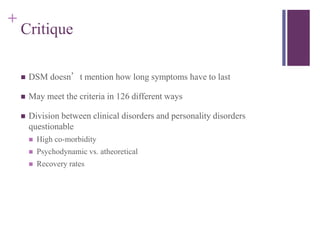
This document provides an overview of personality disorders, including their defining characteristics, diagnostic criteria, prevalence, and treatment approaches. Personality disorders are characterized by inflexible and maladaptive patterns of behavior that cause distress or impairment. They are divided into three clusters (A, B, and C) based on clinical characteristics. Borderline personality disorder is one of the most common personality disorders and is defined by instability in interpersonal relationships, self-image, and affect. Treatment focuses on establishing therapeutic alliances, managing crises, education, and therapies like dialectical behavior therapy that target affect regulation and adaptive coping skills.