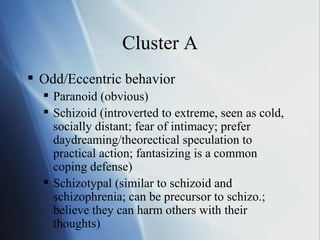
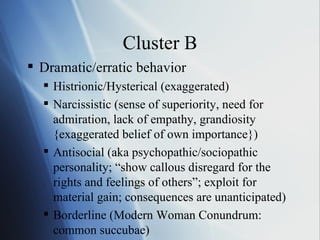
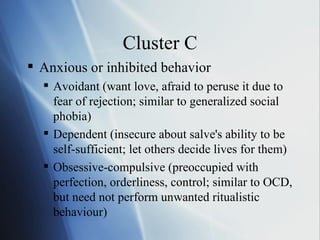
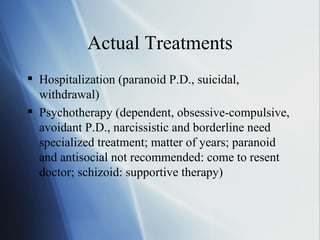
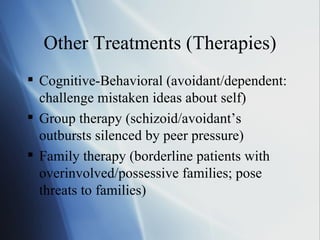
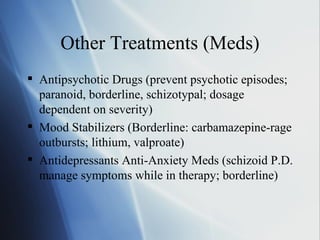
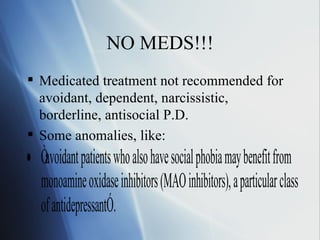
Personality disorders are rigid and self-destructive patterns of thinking and behaving that fall outside of societal norms. They can develop anytime from childhood through early adulthood. Approximately 15% of Americans are estimated to have a personality disorder. Personality disorders are categorized into three clusters based on patterns of perceiving and relating to others: Cluster A includes odd/eccentric behaviors; Cluster B includes dramatic/erratic behaviors; and Cluster C includes anxious or inhibited behaviors. Treatment involves diagnosis, psychotherapy which can take years, and sometimes medication, though some disorders are not recommended for medication. Recovery requires a willingness to undergo treatment.